County-level, age-adjusted breast cancer mortality rates are negatively tied to the proportion of women screened with mammograms, suggest findings published September 14 in JAMA Network Open.
A team led by Taylor Anderson, PhD, from George Mason University in Fairfax, VA, also found statistically significant positive associations between obesity and breast cancer mortality that were consistent across all U.S. counties. However, they reported that access to factors supporting a healthy lifestyle had varying associations with mortality based on the county that people live in.
“These results suggest that breast cancer mortality in the U.S. can be affected by where individuals live and that more comprehensive and geographically targeted interventions may lead to healthier communities,” Anderson and colleagues wrote.
Breast cancer mortality is complex and can be challenging to measure based on geographic distribution. Adding to this, health disparities seen in breast cancer mortality and incidence are driven by factors that are often interrelated. Typically, studies exploring associations between mortality and geography assume that geographic effects on mortality are static, a phenomenon known as spatial stationarity.
The Anderson team sought to identify geographic variation in the associations of population demographics, environmental, lifestyle, and healthcare access with breast cancer mortality at the U.S. county level via a geospatial cross-sectional study. It used data from the Surveillance, Epidemiology, and End Results (SEER) database.
The researchers completed statistical and spatial analysis by using adjusted mortality rates from 2015 to 2019 for 2,176 U.S. counties. To do so, they used an ordinary least squares (OLS) regression model and a multiscale geographically weighted regression (MGWR) model, which they wrote relaxes the assumption of spatial stationarity. The latter model allows for the association between determinants and breast cancer mortality to vary both across geographic space and at different scales, the researchers wrote.
The team also wrote that these models allowed for the magnitude, direction, and significance of coefficients to change across counties based on geography. It measured associations between detriments of mortality and geographic distribution by standardized coefficient (β).
The researchers found that both models agreed on negative associations between the proportion of adults using screening mammography and breast cancer mortality, and positive associations between obesity and mortality.
Associations between detriments and breast cancer mortality at county level:
| Measure | OLS model | MGWR model |
| Proportion of adults using screening mammography | -1.27 | -1.07 |
| Obesity | 1.21 | 0.72 |
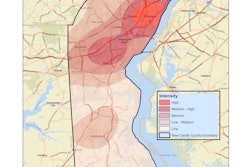
The MGWR model also showed that these determinants were associated with a stationary effect on mortality across the U.S., meaning they share these associations across all U.S. counties included in the study. For mammograms, this effect size is observed in the eastern U.S., with standard coefficients increasing toward positive associations as the data moves toward the western U.S.
Both models also showed negative associations between the following detriments and breast cancer mortality: smoking, food environment index, exercise opportunities, racial segregation, mental health care physician ratio, and primary care physician ratio. They also showed that light pollution had a positive association.
While the OLS model found that these variables are significant factors associated with breast cancer mortality overall, the MGWR model showed that they are only significant in some geographical locations.
“For example, where obesity and mammogram testing have a significant association with mortality in 100% of U.S. counties, smoking had a significant effect in only 16.3%, food environment index in 80.3%, segregation in 22.6%, mental health care physician ratio in 14%, primary care physician ratio in 40.6%, and light pollution in 42.4%,” the study authors wrote.
Inversely, the OLS model found that disability was not a significant variable for breast cancer mortality. However, the MWGR model found that it was significantly positively associated in some geographical locations.
The study authors wrote that these results demonstrate the models tying in place-specific factors with disease-related outcomes and that the MGWR model “brought a novel perspective for capturing the spatial interrelations between individuals and contextual factors on a large geographic scale.”
“As suggested by our analysis, this approach may have an unparalleled ability to identify vulnerable populations and geographic areas where targeted interventions may lead to healthier communities,” they wrote.
The full study can be found here.