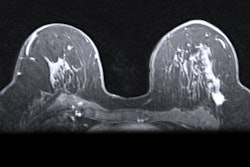
Fewer Black women may meet eligibility criteria for insurance coverage toward supplemental imaging for dense breasts, suggest findings published August 5 in JAMA Network Open.
A team led by Anne Marie McCarthy, PhD, from the University of Pennsylvania in Philadelphia, found that fewer Black women had extremely dense breasts or high lifetime breast cancer risk. It highlighted that a Pennsylvania law’s criteria for supplemental imaging had 0% sensitivity for identifying false-negative mammograms in Black women.
"This means that under the current law, no Black women who later developed cancer after a negative mammogram would have been flagged for supplemental screening," McCarthy told AuntMinnie.
In May 2023, Pennsylvania passed Act 1 of 2023, which mandated that insurance providers must cover supplemental screening for women at increased risk of breast cancer as defined by a set of criteria. One of these criteria points is having dense breasts or a greater than 10% lifetime risk of breast cancer.
While the bill aims to increase screening access for women, the researchers noted that it remains unclear how this law and similar ones passed by other states will affect racial disparities in breast care. They cited previous studies showing that Black women, on average, have a lower overall BI-RADS categorized breast density than white women.
McCarthy and co-authors analyzed the potential differences in eligibility for the Pennsylvania supplemental screening criteria based on breast density between Black and white women. Their cross-sectional study included 68,478 Black and white women, aged 40 to 74 years, who did not have prior breast cancer or known BRCA1/2 variants. The women underwent mammography screening from 2015 to 2021. The team used the Breast Cancer Risk Assessment Tool (BCRAT) to measure lifetime risk.
Of the total women, 38,397 were Black and had an average age of 57 years, while the remaining 30,081 women were white and with an average age of 58 years.
The team reported that fewer Black women had extremely dense breasts and higher lifetime risk compared with white women. Consequently, this led to less Black women meeting the eligibility criteria for insurance coverage.
Comparison between Black, white women for breast density, lifetime risk | |||
Measure | White women | Black women | p-value |
Extremely dense breasts | 5.8% | 2.1% | 0.02 |
≥ 20% lifetime risk | 6.4% | 0.7% | 0.04 |
Women meeting eligibility criteria | 8.4% | 1.6% | 0.02 |
Finally, the team reported that none of the Black women who had a false-negative mammogram met the criteria for supplemental screening, while 36% of white women did.
McCarthy said that breast imaging practices can use this information to critically evaluate current screening protocols and consider more inclusive risk assessment tools.
"Incorporating quantitative breast density measures and body mass index into eligibility criteria may improve sensitivity for detecting cancers in Black women and help reduce disparities in breast cancer outcomes," she told AuntMinnie.
She added that health providers should educate patients about the importance of screening that abides by current guidelines, including reporting and following up on any symptoms as soon as possible, even if the patient recently had a negative mammogram.
"We are currently exploring the impact of incorporating quantitative breast density measurements, polygenic risk scores, and AI models to assess risk for false-negative mammograms as well as risk of breast cancer risk factors," McCarthy said. "We are also evaluating how supplemental screening laws are being implemented in Pennsylvania and the outcomes of those laws."
The full study can be found here.