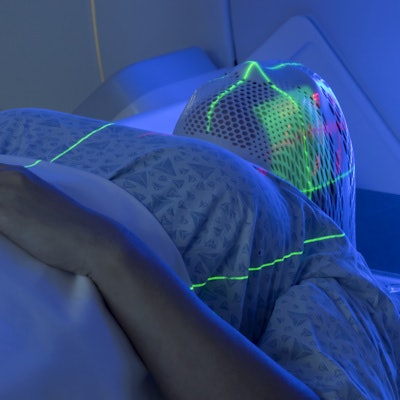
RaySearch Laboratories and Mevion Medical Systems are collaborating to develop advanced treatment planning techniques for delivery of Flash radiation therapy with the Mevion S250i proton therapy system.
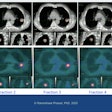
The collaboration will explore Flash intensity-modulated proton therapy delivery using a technique that supports delivering large-volume clinical Flash fields by combining smaller fields. Each field is delivered at Flash dose rates that complement Mevion's Hyperscan delivery system.
Both companies have collaborated previously to provide treatment planning capabilities for Mevion's Hyperscan pencil-beam scanning and Adaptive Aperture pMLC. They will be exhibiting at the upcoming American Society for Radiation Oncology (ASTRO) annual meeting in Chicago, October 24-26.