Ganglioneuroma:
Clinical:
Ganglioneuromas are fully differentiated neuronal tumors composed of large ganglion cells, Schwann cells, and nerve fibers [4]. They are usually attached to either a sympathetic nerve or to an intercostal nerve trunk [4]. The posterior mediastinum is the most common location (41.5% of cases) for this well encapsulated benign lesion arising from sympathetic ganglia composed of mature ganglion cells, Schwann cells, and nerve fibers. Other sites include the retroperitoneum (37%), adrenal gland (20%), and neck [2]. Ganglioneuromas predominantly occur in older children (median age 7 years) and young adults (another article indicated children older than 10 years [4]). There is a male predominance [4]. The lesion tends to be slow growing [4]. Half of the affected patients are asymptomatic. Elevated VMA or HVA levels can be detected in up to 37% of patients [2]. The lesion may accumulate MIBG in up to 57% of cases [2]. The lesion does not metastasize and surgical resection is curative, although local recurrence has been described [2].X-ray:
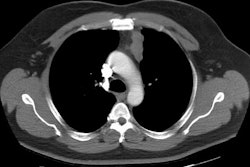
On CT it appears as a well marginated, football shaped, low attenuation mass growing along the axis of the paravertebral chain and it rarely causes any bony changes. The lesion can typically span three to five vertebrae. There is usually slight to moderate contrast enhancement which can be heterogeneous [2]. The lesion tends to partially or completely surround major blood vessels, with little or no compromise of the lumen [3]. Calcification is seen in 20-60% of lesions and usually discrete and punctate [2,3] (other authors indicate the calcification is typically fine and speckled, but can be coarse [4]). Intraspinal extension is seen in only 5%.On MRI, the lesion typically has homogeneous intermediate signal intensity on all sequences [1]. Others describe the most common appearance as low signal on T1 and heterogeneously high on T2 [2]. The T2 signal depends on the proportion of myxoid stroma within the lesion- higher signal on T2 images is associated with a greater amount of myxoid stroma [3]. A "whorled" appearance on T1 or T2, and heterogeneous high signal on T2 images may occasionally be seen.
REFERENCES:
(1) Chest 1997; Strollo DC, et al.
Primary mediastinal tumors. Part II: Tumors of the middle and
posterior mediastinum. 112: 1344-57
(2) Radiographics 2002; Lonergan GF, et al. From the archives of the AFIP. Neuroblastoma, ganglioneuroblastoma, and ganglioneuroma: radiologic-pathologic correlation. 22: 911-934
(3) Radiographics 2003; Rha SE, et al. Neurogenic tumors in the
abdomen: tumor types and imaging characteristics. 23: 29-43
(4) AJR 2016; Pavlus JD, et al. Imaging of thoracic neurogenic
tumors. 207: 552-561