Neuroblastoma
Clinical:
Neuroblastoma is the most common extracranial solid malignant tumor of infants and children. About 50% of cases occur in children less than 2 years of age, and 90% are seen by age 8. Males are affected slightly more than females. Associations with a familial predisposition (0.2%), bowel agangliosis, and CHD have been described, but none are very strong.Symptoms of neuroblastoma include an abdominal mass, limp, nystagmus, or inability to walk. Hypertension is found in 30% of patients. Elevated urinary catecholamine levels (VMA & HVA) are seen in 90%.
Metasases are present in 60% of patients at the time of diagnosis. The skeleton is the most common site (60%). Metastases can also go to lymph nodes (40%), liver, and intracranial (dura). Prognosis is related to patient age (Younger age [esp. under 1 year]->better prognosis), and tumor grade (lower grade or Stage IVs->better prognosis). Occasionally, the lesions may revert to a benign ganglioneuroma (0.2% of cases).
Paraneoplastic syndromes:
- Infantile myoclonic encephalopathy:
- Verner-Morrison syndrome:
associated with occult neuroblastoma in 20-50% of cases, it is the initial presentation of neuroblastoma in about 2% of children. The syndrome consists of opsoclonus (random irregular eye movements or "dancing eyes"), myoclonus,and cerebellar ataxia.
Watery diarrhea, hypokalemia, and achlorhydria. Seen in 5% of cases, it is secondary to VIP production by the tumor (elevated VIP levels are noted in 25% of patients with neuroblastoma).
Sites of Primary Neuroblastoma:
Approximately 75% of cases of neurobalstoma are intraabdominal. The adrenals are the most frequent (50% of cases) intra-abdominal site. About 10% of cases are bilateral. Primary adrenal lesions are actually associated with a worse prognosis than extra-adrenal lesions. Neurobalstoma can also occur in extra-adrenal abdominal sympathetic ganglia which includes the Organ of Zückerkandl (a cluster of paraganglia near the aortic bifurcation, seen predominantly in children). Approximately 15% of cases are intrathoracic. The lesion generally arises posteriorly in the paravertebral sympathetic chain. About 25% will have an associated intraspinal component. Thoracic and cervical primaries are associated with a better prognosis. Primary intracranial neuroblastoma is rare (approximately 2% of cases). It most commonly arises in the olfactory nerve (esthesioneuroblastoma), or cerebellum.Staging of Neuroblastoma
- Stage I: Confined to the organ of origin
- Stage II: Extends into adjacent structures, but does not cross midline. Includes extra-adrenal primaries.
- Stage III: Crosses midline
- Stage IV: Distant metastases
- Stage IVS: Primary lesion does not cross midline, with widespread metastases to liver, skin, and bone marrow (but NOT bone). It is usually seen in infants under 1 year of age. Associated with very good survival following XRT and chemotherapy.
X-ray:
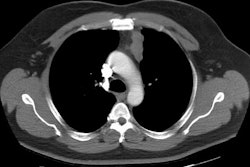
On CT neuroblastoma typically appears as a large complex mass which is often locally invasive into adjacent tissue and typically encases the great vessels, although a pseudocapsule maybe seen. Neuroblastomas often contain areas of necrosis, hemorrhage, and calcification (up to 80%). Calcification can be curvilinear or nodular. The mass may appear cystic and can mimic an adrenal hemorrhage in neonates. Neuroblastomas appear bright on T2-weighted MRI images.Scintigraphy: MIBG scan sensitivity in the detection of neuroblastoma has been reported to be 90% or greater [Seminars, July 93, p.233]. The specificity of MIBG in the detection of neuroblastoma approaches 100%. The extent of metastatic bone and bone marrow disease is most accurately defined by MIBG scintigraphy. Bone scanning often grossly underestimates the extent of osseous metastases (MIBG is superior to MDP for detecting the presence of skeletal metastases). [JNM, Nov.93, p.1922]
Liver metastases may escape detection with MIBG imaging. This finding is not surprising as MIBG is physiologically concentrated in the liver, and therefore small lesions may be obscured. [JNM, Sept.94, p.1434]
SPECT increases diagnostic certainty, but does not increase lesion detection with I123-MIBG [JNM, Nov 1994, 1753]
TcMDP is concentrated in about 2/3 of primary lesions (and is felt to be related to presence of calcification). Bone scan detects the presence of skeletal metastases in 40-60% of patients, but localization of metaphyseal metastases can be difficult due to the adjacent physeal activity. A common finding on bone scan in patients with metaphyseal metastases is ill-defined increased activity in this area with loss of the sharp boundary between the growth plate and the metaphysis.