Minnies finalists, page 2
Best Radiologic Sciences Program
This year's competition features a previous winner and a first-time finalist.
Emory University, Atlanta, GA
 Emory University School of Medicine is in contention for its second Minnie in this category, having previously won in 2018. Its Medical Imaging Program offers students a blend of classroom instruction and direct clinical experience provided by experienced professionals, according to the institution.
Emory University School of Medicine is in contention for its second Minnie in this category, having previously won in 2018. Its Medical Imaging Program offers students a blend of classroom instruction and direct clinical experience provided by experienced professionals, according to the institution.
Students can expect to study anatomy, physiology, and pathology. In addition, they learn image production techniques and patient positioning for acquiring high-quality imaging studies, Emory said. What's more, they train to aid radiologists with image-guided procedures.
Emory offers two pathways to earn a Bachelor of Medical Science (BMSc) degree in its Medical Imaging Program: BMSc and RT-BMSc. The BMSc in Medical Imaging Program is designed for undergraduate students who have no prior training in medical imaging. It includes administration, education, or advanced imaging tracks.
Meanwhile, the RT-BMSc in Medical Imaging Program aims to provide currently credentialed radiographers the opportunity to complete a baccalaureate degree in CT, MRI, radiography education, or radiology administration, according to the university. Online and hybrid course formats are available and the curriculum can be completed on a full-time or part-time basis.
The school has a five-year initial success rate of 82% for students passing the American Registry of Radiologic Technologists (ARRT) exam, as well as a five-year average job placement rate of 100%. And if that isn’t enough, radiologic technologists can sample life outside the clinic or classroom with the city of Atlanta’s many offerings, whether it be sports, the arts, bustling nightlife, or walking and biking trails.
University of Wisconsin, Madison, WI
 Providing remarkable healthcare is an integral part of what's expected from graduates of the University of Wisconsin's (UW) School of Radiologic Technology.
Providing remarkable healthcare is an integral part of what's expected from graduates of the University of Wisconsin's (UW) School of Radiologic Technology.
The school is a hospital-based radiography program sponsored by UW Health University Hospital, and it takes advantage of affiliation agreements with multiple colleges and universities to provide professional medical radiography knowledge to Bachelor of Science in Radiologic Technology (BSRT) candidates. Since 1931, the school has been training tomorrow's radiography graduates to deliver remarkable patient care and advance healthcare through the pillars of service, scholarship, science, and social responsibility, according to UW. The school boasts a five-year credentialing rate of 94% for students passing the American Registry of Radiologic Technologists (ARRT) exam on their first attempt, as well as a five-year average job placement rate of 100%.
Not only are students taught how to obtain medical images and select technical factors, but they also learn about work ethic and professional behavior, developing critical thinking skills in the process, the university said.
However, the school also relies on its students to evaluate the program and find ways the school can improve upon its mission and model for success. The mission, goals, and outcomes endorsed by the UW Health University Hospital School of Radiologic Technology are evaluated annually. Those who participate in the evaluation process include members of the faculty, student body, radiology department, hospital administration, and the School of Radiologic Technology Advisory Committee.
It's through these efforts that UW continues to show success in training aspiring radiographers.
Most Significant News Event in Radiology
Both the tip and the iceberg have been selected by the Minnies expert panel as finalists for the Most Significant News Event in Radiology in 2023 – ChatGPT, specifically, and the use of AI in radiology took the top two spots.
ChatGPT attracts interest for potential radiology applications
 In just 10 months since its launch on November 30, 2022, radiologists have tested ChatGPT in tasks ranging from helping lift the burden of preauthorizations to taking radiology board exams.
In just 10 months since its launch on November 30, 2022, radiologists have tested ChatGPT in tasks ranging from helping lift the burden of preauthorizations to taking radiology board exams.
Our first story was published on January 26, based on an editorial in Radiology that pegged Open.AI's large language model (LLM) as a double-edged sword. A team at New York University (NYU) noted the technology's potential strengths for clinicians and patients but warned of its "hallucination effect," namely its ability to produce seemingly credible but incorrect responses.
These hallucinations, as they are now simply called, so far appear to be an Achilles' heel of the chatbot in terms of its use as a clinical tool for radiologists, yet other studies have revealed ChatGPT's more realistic potential to help educate patients. Recently, for instance, a team in Germany recommended using ChatGPT to help prepare patients for PET/CT scans.
So, will ChatGPT be the smartest doctor in the world one day? For one radiology expert's opinion on this question, check out our interview with Rajesh Bhayana, MD, of the University of Toronto.
AI in radiology
 The last time AI in radiology was named the Most Significant News Event in Radiology was 2019 (its fourth straight year), with the COVID-19 pandemic dominating the top spot for the past three years.
The last time AI in radiology was named the Most Significant News Event in Radiology was 2019 (its fourth straight year), with the COVID-19 pandemic dominating the top spot for the past three years.
With new algorithms approved by the U.S. Food and Drug Administration (FDA) seemingly on a weekly basis, there's no doubt the technology is continuing to have a significant impact on radiology. One estimate suggests the medical imaging AI market is expected to exceed $1.7 billion by 2027.
Even in nuclear medicine, AI applications appear to be picking up steam, with experts recently discussing whether or not AI algorithms will eventually replace conventional radiomics analysis.
AuntMinnie's coverage of discussions at the annual meeting of the Society for Imaging Informatics in Medicine in June provided an excellent snapshot of the technology's current status. Questions seem to have shifted from "How does AI work?" to "How can AI work for me?"
In one interview, for instance, Marc Kohli, MD, of the University of California, San Francisco, tackled a popular question: How can practices trust the AI technology they want to implement?
These questions aside, early research has begun to suggest that patient attitudes may be shifting in a positive way toward the technology. Researchers in the U.K. recently characterized patient responses gleaned in focus groups by stating that most think implementing AI "sounds like a brilliant idea."
So, will AI be returning to the winning circle this year in the category of the Most Significant News Event in Radiology? Stay tuned to find out.
Biggest Threat to Radiology
Workforce shortages
 For years, professional organizations have been sounding the alarm that the U.S. will soon be facing a physician shortage that will threaten patient access to care. This year has been no different: In March, the American College of Radiology (ACR) and the Radiology Business Management Association (RBMA) sent a letter to the U.S. Senate Committee on Health, Education, Labor, and Pensions (HELP) that highlighted a 2021 report from the Association of American Medical Colleges (AAMC) projecting that by 2034, the U.S. could face a shortage of between 37,800 and 124,000 physicians, with shortages in other specialties -- including radiology -- ranging from 10,300 to 35,600 physicians. And in May, the American Society of Radiologic Technologists (ASRT) released a report that found a radiologic technologist (RT) vacancy rate of 18.1% this year. Also that month, the American Society for Radiation Oncology (ASTRO) held an Advocacy Day in Washington, DC, urging its members to educate Congress about how staffing shortages negatively affect patient care in cancer clinics and to ask for policies that would decrease these shortages.
For years, professional organizations have been sounding the alarm that the U.S. will soon be facing a physician shortage that will threaten patient access to care. This year has been no different: In March, the American College of Radiology (ACR) and the Radiology Business Management Association (RBMA) sent a letter to the U.S. Senate Committee on Health, Education, Labor, and Pensions (HELP) that highlighted a 2021 report from the Association of American Medical Colleges (AAMC) projecting that by 2034, the U.S. could face a shortage of between 37,800 and 124,000 physicians, with shortages in other specialties -- including radiology -- ranging from 10,300 to 35,600 physicians. And in May, the American Society of Radiologic Technologists (ASRT) released a report that found a radiologic technologist (RT) vacancy rate of 18.1% this year. Also that month, the American Society for Radiation Oncology (ASTRO) held an Advocacy Day in Washington, DC, urging its members to educate Congress about how staffing shortages negatively affect patient care in cancer clinics and to ask for policies that would decrease these shortages.
What's contributing to the threat in radiology? The impending retirement of older radiologists could be a factor, but staff shortages may also be influenced by a rapid increase in the need for medical imaging as the U.S. population ages and incidence of chronic diseases continues to rise -- in fact, some experts have estimated that the U.S. imaging market's compound annual growth rate (CAGR) will increase by 4.2% between 2022 and 2030 -- and the number of available radiologists just won't be able to fill the gap.
But there may be help on the horizon in the form of revamping work protocols to include remote or hybrid strategies and incorporating AI into a department's workflow to make not only image interpretation but also patient exams more efficient.
Burnout among physicians and staff
 Physician and staff burnout has been called the biggest threat to radiology by the Minnies expert panel since 2019 -- it won the category last year -- and once again, it's making it into the semifinal round. The problem is ubiquitous: In 2022, a Medscape survey found that 49% of radiologists reported feeling burnt out, and 54% to 72% reported symptoms of the condition.
Physician and staff burnout has been called the biggest threat to radiology by the Minnies expert panel since 2019 -- it won the category last year -- and once again, it's making it into the semifinal round. The problem is ubiquitous: In 2022, a Medscape survey found that 49% of radiologists reported feeling burnt out, and 54% to 72% reported symptoms of the condition.
There are a number of ideas for mitigating burnout, including enabling radiologists' professional development, implementing remote work protocols, and helping radiologists cope with moral distress (that is, the conflict that arises when a clinician knows the right course of action but institutional constraints make it difficult to choose). In any case, the problem of burnout in radiology is a thorny one and will likely continue to challenge radiology staff, from administrators and technologists to radiologists themselves.
Hottest Clinical Procedure
Photon-counting CT
 Will photon-counting CT (PCCT) take the top spot in the Minnies Hottest Clinical Procedure category for a third straight year?
Will photon-counting CT (PCCT) take the top spot in the Minnies Hottest Clinical Procedure category for a third straight year?
According to proponents, the procedure is "the first new quantum leap in CT technology in a decade," with benefits including ultrahigh spatial resolution of the lung parenchyma using small detector pixels, higher matrix size, thinner slice thickness – as low as 0.15 mm – and higher frequency filters.
Essentially, PCCT directly captures x-ray photons as electric signals without having to then convert them to light, as conventional CT has to do. This capability translates to better spatial resolution, higher iodine image contrast, and better radiation dose efficiency, studies suggest.
While the technology does have a forerunner in dual-source, dual-energy CT, PCCT ultimately may expand the modality's capability by adding spectral imaging and ultrahigh resolution to the tool kit, researchers suggest.
The technology took top headlines at the International Society of Computed Tomography ISCT 2023 meeting in San Diego, with studies clarifying its clinical benefits, and researchers at ECR 2023 in Vienna also singing its praises.
Use of AI for predictions
 This is the first time the Minnies expert panel has nominated AI in the Hottest Clinical Procedure category. Can it be that this pairs with the category Biggest Threat to Radiology, where physician burnout has reigned for four years?
This is the first time the Minnies expert panel has nominated AI in the Hottest Clinical Procedure category. Can it be that this pairs with the category Biggest Threat to Radiology, where physician burnout has reigned for four years?
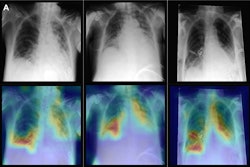
In other words, clinical studies have hit their stride in 2023 in terms of evaluating AI algorithms in clinical settings, primarily as aids to mitigate burnout. Tellingly, this is despite studies showing that the many claims advertised by developers aren't supported by publicly published data.
There's certainly no shortage of algorithms to evaluate. In neuroimaging alone, the U.S. Food and Drug Administration has currently cleared at least 59 algorithms: 24 are compatible with noncontrast CT, 21 with MRI, nine with CT perfusion, eight with CT angiography, three with MR perfusion, and two with PET. Six algorithms are compatible with multiple imaging techniques.
Yet studies evaluating AI chest x-ray algorithms may be where the rubber meets the road, with developers able to leverage larger patient datasets than with other modalities. In one study, for instance, researchers used chest x-rays from 7,105 patients to develop a deep-learning model that predicts 30-day mortality in patients with community-acquired pneumonia.
In another study, an AI algorithm designed for SPECT heart imaging predicted potentially fatal events in patients with cardiovascular artery disease.
Will this first-time nomination be the charm for predictive AI as the Hottest Clinical Procedure? Stay tuned to find out what the Minnies panel decides.
Continue reading: Back to Page 1, Page 3.













![Images show the pectoralis muscles of a healthy male individual who never smoked (age, 66 years; height, 178 cm; body mass index [BMI, calculated as weight in kilograms divided by height in meters squared], 28.4; number of cigarette pack-years, 0; forced expiratory volume in 1 second [FEV1], 97.6% predicted; FEV1: forced vital capacity [FVC] ratio, 0.71; pectoralis muscle area [PMA], 59.4 cm2; pectoralis muscle volume [PMV], 764 cm3) and a male individual with a smoking history and chronic obstructive pulmonary disorder (COPD) (age, 66 years; height, 178 cm; BMI, 27.5; number of cigarette pack-years, 43.2, FEV1, 48% predicted; FEV1:FVC, 0.56; PMA, 35 cm2; PMV, 480.8 cm3) from the Canadian Cohort Obstructive Lung Disease (i.e., CanCOLD) study. The CT image is shown in the axial plane. The PMV is automatically extracted using the developed deep learning model and overlayed onto the lungs for visual clarity.](https://img.auntminnie.com/mindful/smg/workspaces/default/uploads/2026/03/genkin.25LqljVF0y.jpg?auto=format%2Ccompress&crop=focalpoint&fit=crop&h=112&q=70&w=112)