SAN FRANCISCO - Having shown the feasibility of real-time, 3D echocardiography-guided cardiac surgery without cardiopulmonary bypass, Boston-based surgeons tested the technique in atrial septum defect (ASD) closure. Dr. Yoshihiro Suematsu shared their results Wednesday at the American Association for Thoracic Surgery (AATS) meeting.
"This (technique) has great potential for expanding applications, not only for medical diagnosis, but also for image-guided intervention," Suematsu said.
Suematsu and co-authors are from the Children's Hospital Boston, Boston University, and Harvard Medical School. This presentation built on previous research by this group. Last year, they described real-time 3D echocardiography (RT3DE) with specialized instrumentation to facilitate beating-heart repair of atrial septal defects and mitral valve plasty. In two feasibility studies, they concluded that echo "provides adequate imaging and anatomic detail to act as a sole guide for surgical task performance" (Journal of Thoracic and Cardiovascular Surgery, October 2004, Vol. 128:4, pp. 579-587; July 2004, Vol. 128:1, pp. 53-59).
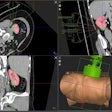
For this animal experiment, a modified RT3DE system with a 2- to 4-MHz transducer was used to guide surgery (Sonos 7500, Philips Medical Systems, Andover, MA). Eighteen swine were anesthetized and, after median sternotomy, the echo probe was applied directly to the surface of the right atrium.
Balloon atrial septectomy and enlargement of the ASD were performed through a purse-string suture on the right atrial appendage. Three different techniques for ASD closure were used:
- Direct suture closure with semiautomatic suturing device
- Amplatzer ASD device closure
- Patch closure with 5-mm endoscopic stapler
The results showed that RT3DE provided sufficient spatial resolution and frame rate, offering a "virtual surgeon's view" of the relevant anatomy throughout the procedure. All the atrial septal defects were enlarged without collateral injury, and the final size of ASD was 8.5 ± 1.8 mm in diameter. All surgical techniques for ASD closure were successfully performed under RT3DE guidance. Intraoperative 2D color Doppler echocardiography and postmortem macroevaluation revealed no residual shunts.
"RT3DE-guided beating-heart ASD closure is feasible. Unlike catheter devices, it is applicable for any type of secundum ASD," Suematsu concluded. "In the future, with the advent of 3D transesophageal echo probes, this procedure may even be performed without medial sternotomy with portal access."
In an invited AATS commentary, Dr. Ludwig von Segesser from Centre Hospitalier Universitaire Vaudois in Lausanne, Switzerland, pointed out that his group performed a similar procedure back in 2003, but had to rely on two different intravascular ultrasound systems in order to produce a 3D image.
"There can be no doubt that the 3D imaging presented here is a major progress compared to the previous technique," von Segesser said. He asked Suematsu how his team handled the tricky task of capturing moving targets on 3D echo and whether they used valve leaflets.
Suematsu said they relied on 3D echo-guidance for their ventricular approach and also used endoscopic forceps. He reiterated that improved, high-frequency 3D echo probes would be required to continue to advance this technique.
By Shalmali Pal
AuntMinnie.com staff writer
April 13, 2005
Related Reading
MRI pulls double duty for PFO, atrial septal aneurysm, January 14, 2005
Copyright © 2005 AuntMinnie.com