Anal fissures -- tears in the skin that can be slow to heal -- respond well to treatment with botulinum toxin, and delivering the drug with the aid of endoscopy makes the procedure easier and safer, according to a Chicago-area doctor.
Dr. Eli Ehrenpreis from Northwest Community Hospital in Arlington Heights, IL said he relies on endoscopy to precisely locate the internal anal sphincter so that the injection of botulinum toxin type A (Botox) can be accurately administered.
Currently, most physicians use a blind insertion of the needle into the internal anal sphincter, a method that causes considerable pain to the patient, imprecise medication delivery, and the potential for needle-stick injury to the physician, he said.
"We have only a few patients in this pilot study, but we think the information is practical and can be used immediately by other doctors. Anal fissure is a condition that occurs frequently and affects a wide range of patients," said Ehrenpreis during a talk at Digestive Disease Week 2003 in Orlando, FL.
The condition, which occurs more often in elderly individuals who suffer from constipation, can develop in just about anyone. Chronic anal fissures result from a learned habit of straining, which makes it difficult for the fissures to heal normally. Muscle spasms, which prevent blood flow to the wound, and the presence of bacteria slow healing, Ehrenpreis explained. When botulinum toxin type A is injected into the internal anal sphincter, the structure relaxes so that a patient can defecate without straining.
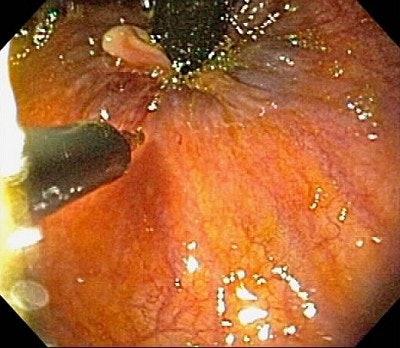 |
| Endoscopic injection of Botox into the internal anal sphincter in a patient with a chronic anal fissure. An upper endoscope is placed in a retroflexed position after cleansing of the distal rectum with Betadyne. The injection is performed near the dentate line (junction of anal and rectal mucosa) using a sclerotherapy needle. Image courtesy of Dr. Eli Ehrenpreis. |
In this series the 10 patients ranged in age from 25 to 84. The procedure consisted of an upper endoscope inserted into the rectum and placed in the retroflexed position. This was followed by standard sigmoidoscopy preparation. Thirty cubic centimeters of 10% iodine solution was used to flush the area proximal to the dentate line.
"We injected 100 units of Botox with a sclerotherapy needle into the internal anal sphincter just proximal and lateral to the dentate line which is clearly visible with the endoscope," he explained. Eight out of 10 patients have experienced complete resolution of the condition after endoscopically-guided Botox treatment.
Ehrenpreis said that one major concern of treatment is the possibility of fecal incontinence, but that none of the patients in his study suffered from that condition. And any incontinence would be short-term as the Botox treatment wears off after a few months, he said.
Another 10 patients have undergone the procedure since Ehrenpreis prepared his initial report. Several patients required a second injection of Botox before their condition resolved. One patient did require surgery; another developed an acute anal fissure, which also was repaired surgically.
In addition to the anal sphincter patients, Ehrenpreis said he uses the technique on patients with nonrelaxing puborectalis syndrome.
"I am now doing about one of these endoscopic procedures a week," he said.
By Edward SusmanAuntMinnie.com contributing writer
June 18, 2003
Related Reading
PointDx signs SPIn-DR, June 2, 2003
'Fantastic voyage' into gut nearer to reality, May 21, 2003
Post-toilet cystoproctography pinpoints enteroceles of small bowel, May 9, 2003
Needlestick injuries: A "silent epidemic" in radiology, April 19, 2002
Copyright © 2003 AuntMinnie.com