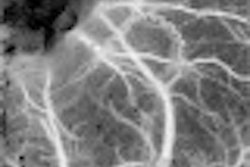
SAN FRANCISCO - Ultrasound angiography offers top-notch intraoperative guidance during arteriovenous malformation (AVM) surgery, according to a poster presentation Tuesday at the Congress of Neurological Surgeons (CNS) meeting.
"Preoperative MR angiography (MRA) and intraoperative ultrasound angiography of AVMs are presented as stereoscopic images on the monitor ... (by) a simple red/blue technique," Dr. Geirmund Unsgård, Ph.D., and Frank Lindseth, Ph.D., wrote in their poster. "Due to integration with a navigation system, it is possible to identify larger vessels...."
Unsgård is from St. Olav's Hospital and the Norwegian University of Science and Technology in Trondheim, Norway. Lindseth is from Trondheim-based Sintef Health Research, the company that developed the ultrasound angiography technology.
"One objective (of the study) was to see how it could help us understand the (angiographic) architecture of the AVM," Unsgård said during a discussion of the poster. "The other was to help us identify and clip the AVM at an early phase of the operation."
The study involved 11 patients and used SonoWand (Mison, Trondheim, Norway), a system that integrates 3D ultrasound and navigation. A stereoscopic pointer allows for the identification of larger vessels.
The patients ranged in age from 19-52, and were given Spetzler-Martin grades for AVM ranging from II to IV. Their symptoms included headache, dizziness, syncope, visual disturbance, and epilepsy. AVMs were localized in the right parietal lobe in three patients, in the left parietal lobe in three patients, two each in the left and right occipital lobes, and one in the left frontal lobe.
Of the 28 arteries feeding the AVM (referred to as feeders) identified on the preoperative sonographic images, 25 could be clipped at the start of surgery. Three others were clipped at a later stage of surgery because they were located behind the AVM, Unsgård said.
Early clipping of the feeders made the surgery easier to perform, the authors said, and ultrasound angiography even identified residual AVM vessels that were subsequently removed.
The method was particularly useful for brain-shift correction and nidus visualization, they said. In one example, the pointer tip was placed on the vessel, but the stereoscopic view on MRA placed the localization dot above the target vessel. On the other hand, the "dot" defined by ultrasound angiography was more specific and closer to the vessel.
After treatment, only one patient acquired a permanent neurological deficit. Of the 11 patients, five showed normal function at follow-up, one developed epilepsy, and one had no change in visual disturbance after the procedure, but did not have any postsurgical complications.
"The (ultrasound angiography) technology makes it easier to understand the vascular architecture during the operation, and it offers a possibility to identify and clip AVM feeders both on the surface and deep in the tissue at the beginning of the operation," the authors stated.
This ultrasound-guided method "enhances the surgeon's perception of the vascular architecture," Unsgård said. "My experience is that the technology makes it easier and probably safer to remove the AVM because you ... have all the major feeders," he added. He also acknowledged that a larger clinical study was necessary to further evaluate this technique.
The Norwegians' results bolster previous studies involving ultrasound guidance for AVM surgery. In a case report, neurosurgeons from Ondokuzmayis University in Samsun, Turkey, successfully used intraoperative grayscale ultrasound to localize AVM, identify the feeders, note perilesional changes, and detect accompanying hematomas (Minimally Invasive Neurosurgery, June 2003, Vol. 46:3, pp. 169-172).
More recently, a group from the University of Wisconsin in Madison used spectral Doppler to distinguish feeding arteries from en passant and normal vessels in patients undergoing AVM resection. They also found that duplex Doppler allowed more accurate localization of the AVM nidus, and indicated the completeness of resection (Neurosurgery, July 2004, Vol. 55:1, pp. 155-160).
By Shalmali Pal
AuntMinnie.com staff writer
October 21, 2004
Related Reading
Cuban radiologists rely on transcranial ultrasound, July 4, 2002
MRI accurately assesses angiodysplasia, May 25, 2002
Copyright © 2004 AuntMinnie.com