Bronchiolitis / Constrictive Bronchiolitis:
View cases of bronchiolitis
Clinical:
Bronchiolitis refers to a group of disorders which affect the
small airways. Small airways are defined as non-cartilagenous
airways with an internal diameter of 2-3 mm or less and are
located from approximately the eighth generation of airways down
to the terminal bronchioles (which are the smallest airways
without alveoli), the respiratory bronchioles (which are the
airways distal to the terminal bronchioles that partake in gas
exchange), and the alveolar ducts) [6,7,12]. Bronchiolitis can be
further classsified as constrictive or proliferative/cellular
[7,9,13]. In proliferative bronchiolitis there is organizing
intraluminal exudate within the airways [9]. Proliferative
bronchiolitis can be idiopathic, or associated with infection,
aspiration, collagen vascular disease (especially
dermatomyositis), hypersensitivity pneumonitis, and eosinophilic
pneumonia [9]. Acute infectious bronchiolitis is the most common
type of bronchiolitis and is typically viral (RSV or
parainfluenza) or bacterial (Mycoplasma or S. aureus)
[13]. Chronic infectious bronchiolitis is frequently mycobacterial
or Pseudomonas in etiology [13].
Cyrptogenic bronchiolitis with organizing pneumonia (COP) was previously referred to as BOOP. COP represents a proliferative bronchiolitis associated with organizing pneumonia in the surrounding lung parenchyma. (see discussion of "COP/BOOP" in the Autoimmune Section)
In constrictive bronchiolitis, non-specific inflammation of the bronchiole wall eventually leads to fibrosis with narrowing or obstruction of the bronchiolar lumen, but the surrounding lung parenchyma is normal and there is no intraluminal granulation tissue or polyps [10]. The terms obliterative bronchiolitis and bronchiolitis obliterans are synonymous with constrictive bronchiolitis [7]. Clinically patients have evidence of irreversible airflow obstruction, in particular, a marked reduction in air flow at low lung volumes. The severity of chronic airflow obstruction is proportional to the extent of bronchioles involved and their degree of narrowing [7]. Symptoms are relatively non-specific with shortness of breath and cough. Etiologies for constrictive (obliterative) bronchiolitis include:
1. Infectious: CMV, TB (endobronchial spread), mycoplasma or viral infections (adenovirus 7 and 21) in childhood, or respiratory syncitial virus in young adults.
2. Non-infectious:
i. Organ transplant patients:
Graft versus host disease (bone marrow transplant) or lung transplant. Bronchiolitis obliterans in lung transplant patients is though to be a manifestation of chronic allograft rejection, occurring in up to 50% of long term lung transplant survivors. The associated finding of bronchiectasis is noted in 67% of transplant patients with bronchiolitis obliterans [1].
ii. Collagen vascular disease: Rheumatoid arthritis and polymyositis
iii. Inhaled toxins/inhalational injury: Sulfur dioxide, ammonia, chlorine, phosgene, nitrogen dioxide (silo filler's lung), and ozone.
iv. Drugs: Penicillamine [10] and sulfasalazine [11].
v. Idiopathic (Primary): A chronic respiratory illness characterized by chronic cough, dyspnea, obstructive physiology, relatively normal CXR, and a lack of response to bronchodilators or prednisone [6]. The condition mainly affects women between the ages of 40 to 60 years.
Diffuse panbronchiolitis and respiratory bronchiolitis represent other forms of bronchiolitis and are discussed elsewhere (see Diffuse Panbronchiolitis and Respiratory Bronchiolitis in Autoimmune section)
X-ray:
Proliferative bronchiolitis: In the typical form of proliferative bronchiolitis there are ill-defined centrilobular micronodules on HRCT which produce a "tree and bud" pattern. There may or may not be associated thickening of the secondary interlobular septae. Other findings include ground glass opacities, acinar nodules, and bronchiole dilatation and wall thickening.
Constrictive bronchiolitis: Plain films are insensitive for the
diagnosis of bronchiolitis obliterans and can be normal in 30-40%
of cases. When abnormal, the findings are often subtle such as
mild hyperinflation or peripheral attenuation of the vascular
markings.
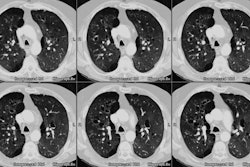
Abnormal findings are more evident on HRCT and can be identified
in up to 90% of cases. Constrictive bronchiolitis typically has a
patchy distribution throughout both lungs. There will be a
heterogeneous density or mosaic attenuation pattern within the
lungs due to air trapping (due to obstruction of the lumen of the
respiratory bronchioles and alveolar ducts) and reflexive
vasoconstriction (due to decreased ventilation) that can be
confirmed on expiratory images. As a result, the lung parenchyma
will demonstrate areas of decreased attenuation with small
vessels, and areas of increased attenuation with enlarged vessels.
Heterogeneous attenuation can be identified in 83-87% of cases. In
13% to 50% of cases, inspiratory images will be normal and
heterogeneous attenuation will only be evident on expiratory
images [8]. Bronchiectasis is a common finding, but need not be
present for the diagnosis [4]. Less commonly, the presence of
centrilobular branching structures or nodules can be noted. [2,3].
Note that mild mosaic attenuation can be seen in up to 20% of
normal patients on inspiratory images and lobular air trapping
occurs in 40-80% of patients on expiratory images [12]. In
general, mosaic attenuation or airtrapping involving more than a
pulmonary segment often has an underlying pathologic basis [12].
REFERENCES:
(1) J Thorac Imag 1995, 10: 236-254
(3) Radiology 1997; 203: 721-726
(5) Chest 1983; Seggev JS et al. Bronchiolitis obliterans: Report of three cases with detailed physiologic studies. 83 (2): 169-174
(6) Radiol Clin North Am 1998; Stulbarg MS, et al. Obstructive pulmonary disease: The clinician's perspective. 36 (1): 1-13
(7) Radiol Clin North Am 1998; Worthy SA, et al. Small airways disease. 36 (1): 163-173
(8) AJR 1998; Arakawa H, et al. Air trapping on expiratory high-resolution CT scans in the presence of inspiratory scan abnormalities: Correlation with pulmonary function tests and differential diagnosis. 170: 1349-1353
(9) AJR 1994; Garg K, et al. Proliferative and constrictive bronchiolitis: Classification and radiologic features. 162: 803-808
(10) AJR 2005; Pipavath SJ, et al. Radiologic and pathologic features of bronchiolitis. 185: 354-363
(11) Radiol Clin N Am 2005; Lindell RM, Hartman TE. Chest imaging
in iatrogenic respiratory disease. 43: 601-610
(12) Radiographics 2015; Kligerman SJ, et al. Mosaic attenuation:
etiology, methods of differentiation, and pitfalls. 35: 1360-1380
(13) Radiographics 2017; Winningham PJ, et al. Bronchiolitis: a
practical approach for the general radiologist. 37: 777-794