Breast imaging surveillance should be tailored for differences in locoregional recurrence patterns according to cancer subtypes, a South Korean study published June 21 in JAMA Surgery found.
Researchers led by Jong-Ho Cheun, MD, from Seoul Metropolitan Government-Seoul National University Boramae Medical Center found that locoregional breast cancer recurrence appears in different patterns according to cancer subtypes. They also concluded that younger women show greater differences in patterns among subtypes than older women.
"Knowledge of the recurrence pattern may help identify the periods of prevalent breast cancer recurrence and optimize the surveillance strategy," Cheun and co-authors wrote.
Early treatment of locoregional recurrence after initial breast cancer treatment is tied to improved prognosis. This makes annual imaging surveillance via mammography important for women in this population. It also makes tumor subtype identification important to guide treatment strategies.
However, the researchers noted that current "major" guidelines don't include tailored surveillance strategies that account for tumor subtypes after surgery. They also pointed out that "few" studies report annual patterns of locoregional recurrence for rumor subtypes.
Using retrospective data, Cheun and colleagues wanted to explore such patterns for ipsilateral breast tumor recurrence, regional recurrence, and contralateral breast cancer. They included data from 16,462 women with a median age of 49 years at the time of operation. The women underwent mammography and breast sonography with a median interval of 12 months and 10.1 months, respectively.
The team reported that the 10-year survival rates for each cancer type were the following: ipsilateral breast tumor recurrence, 95.9%; regional recurrence, 96.1%; and contralateral breast cancer, 96.5%.
Also, HR-/ERBB2+ tumors had the worst ipsilateral recurrence-free survival, with an adjusted odds ratio (OR) of 2.95 versus HR+/ERBB2- tumors. The team also reported that the HR-/ERBB2- subtype had the worst regional recurrence-free and contralateral breast cancer-free survival among all subtypes. This included adjusted OR values of 2.95 and 2.12 versus the HR+/ERBB2- subtype.
The researchers also found that ipsilateral recurrence patterns of HR-/ERBB2+ and HR-/ERBB2- subtypes showed double peaks, while HR+/ERBB2- tumors showed a "steadily increasing pattern" without identifiable peaks. They added that the HR+/ERBB2- subtype "seemed to have a steady regional recurrence pattern." However, they also found that other subtypes showed the highest regional recurrence incidence at one year following surgery, which then gradually decreased.
The team also reported that the annual recurrence of contralateral breast cancer "gradually increased" among all subtypes. Also, women with the HR-/ERBB2- subtype had a higher incidence than women with other subtypes over a 10-year period.
Finally, the researchers found that younger women (40 years or younger) had greater differences in recurrence patterns between subtypes than what was found in older women. For example, younger women experienced a higher incidence of double peaks for annual ipsilateral recurrence incidence than in older women, "especially" for the HR-/ERBB2+ subtype. Also, the incidence of regional recurrence decreased during the first five years for younger women, and all subtypes except the HR-/ERBB2- subtype showed a rebounded increasing pattern afterward.
The study authors suggested that more frequent surveillance may be recommended for younger women. They also called for multi-institutional studies with larger datasets to generalize their findings.
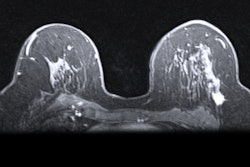
In an accompanying editorial, researchers led by Chelsea Marin, MD, from the University of Rochester in New York wrote that breast MRI may be a suitable imaging surveillance method for certain women.
"We advocate for a data-driven and unified approach to determining which patients should receive breast MRI as part of their surveillance regimen after a breast cancer diagnosis," Marin and colleagues wrote. "Young patients with HR-/ERBB2+ or triple-negative breast cancer may benefit from the addition of breast MRI as part of their surveillance in the first two to three years after surgery."