Most young women who are diagnosed with breast cancer had no prior imaging performed, according to research presented May 1 at the American Roentgen Ray Society (ARRS) annual meeting in San Diego, CA.
In her presentation, medical student Dana Kong from Case Western Reserve University in Cleveland, OH, shared results from her team’s study, which also showed that ultrasound and diagnostic mammography are the most used modalities in diagnosing women ages 40 years or younger.
“We believe our project is a jumping-off point that supports the conclusion that the assessment of utilization patterns of breast imaging services in this population can improve understanding regarding the role and impact of imaging on cancer diagnosis and outcomes,” Kong said.
Recent reports suggest that breast cancer incidence rates are rising among women who are younger than the age ranges recommended for annual screening by medical societies. Younger women tend to be diagnosed at later stages with more aggressive cancers and are more likely to carry genetic mutations.
For women under 40 years of age, breast cancer screening is not considered or available. The American College of Radiology (ACR) does not recommend breast cancer screening for average-risk women under 40 years. But for high-risk women, it does recommend annual MRI surveillance starting from ages 25 to 30 and annual screening mammography for women ages 25 to 40 years depending on risk type.
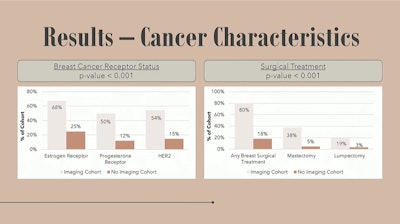 At ARRS 2025, Dana Kong from Case Western Reserve University presented on breast cancer trends among women aged 40 years and younger. Among her team's findings, young women who had imaging prior to their cancer diagnosis had higher receptor status and underwent surgery more frequently than those with no prior imaging.ARRS
At ARRS 2025, Dana Kong from Case Western Reserve University presented on breast cancer trends among women aged 40 years and younger. Among her team's findings, young women who had imaging prior to their cancer diagnosis had higher receptor status and underwent surgery more frequently than those with no prior imaging.ARRS
Kong and colleagues studied the prevalence, demographic characteristics, and clinical characteristics of breast cancer in women aged 40 and younger. They also evaluated the use of breast imaging modalities prior to diagnosis in these women.
The team gathered data collected between 2005 and 2025 from a federated research network containing deidentified patient data (TriNetX). This included 92 healthcare organizations across five countries, with nearly 69.5 million female patients and nearly 1.3 million women with a breast cancer diagnosis.
From there, the researchers identified 82,586 women with breast cancer diagnosed at or below age 40. This represented 0.1% of the total women and 6.5% of female breast cancers. The researchers divided the women into two groups: those who received breast imaging exams at least six months prior to diagnosis (n = 14,426) and those who did not receive imaging (n = 67,951).
The team reported the following:
- Diagnostic ultrasound was the most-used imaging modality in women ages 40 and under, with diagnostic mammography next at 62%.
- The average age at diagnosis was 35.6 years in the imaging cohort and 34.8 years in nonimaging cohort (p < 0.001).
- Women in the imaging cohort, when compared with the nonimaging cohort, were more likely to identify as white (64% vs. 49%) or Black/African American (14% vs. 10%) and not Hispanic or Latino ethnicity (64% vs. 48%).
The team also found that women in the imaging cohort had higher estrogen receptor, progesterone receptor, and HER2 expression than the nonimaging cohort. And the imaging cohort more often underwent surgery.
Comparison of genetic mutations and treatment between women ages 40 and younger who had imaging performed 6 months prior to breast cancer diagnosis | ||
| Nonimaging cohort | Imaging cohort |
Estrogen receptor | 25% | 68% |
Progesterone receptor | 12% | 50% |
HER2 expression | 15% | 54% |
Surgical treatment | 18% | 80% |
Kong highlighted that while surgical treatments were different between the imaging and nonimaging cohorts, this may be related to inherent differences and risks between the two groups.
Kong said that future directions for research include extracting clinical characteristics and risk factors and assessing trends of cancer diagnosis and outcomes. She added that the team plans to compare breast imaging use between the U.S. and other regions around the world.
“We believe this represents an opportunity in imaging to encourage young women to get their recommended risk assessment, as well as an opportunity to provide education on what to look out for,” she said.