Patients that receive a substandard ultrasound visualization score have a higher risk of developing hepatocellular carcinoma (HCC), according to research published May 30 in Radiology.
Researchers led by Min Kyung Park, MD, PhD, from Seoul National University also found that these patients have higher odds of false-negative rates of ultrasound for detecting HCC than those with a good ultrasound Liver Imaging Reporting and Data System (LI-RADS) visualization score.
"These findings suggest that the baseline ultrasound visualization score remains a relevant indicator for predicting the risk of subsequent HCC and can be used to assess the diagnostic performance of ultrasound surveillance for detecting HCC," Park and colleagues wrote.
Ultrasound is the go-to surveillance imaging method for HCC cases. However, the researchers pointed out that ultrasound's success depends on the degree of fibrosis or steatosis, as well as the causes of liver disease.
Park and colleagues wanted to investigate ultrasound's detection power and HCC occurrence, using the ultrasound LI-RADS visualization score in patients with chronic hepatitis B. LI-RADS proposes three levels of visualization scoring that depends on the degree of limitation. Visualization A means no or minimal limitations, visualization B indicates moderate limitations that may obscure small masses, and visualization C means severe limitations that would significantly lower the sensitivity of detecting focal liver lesions.
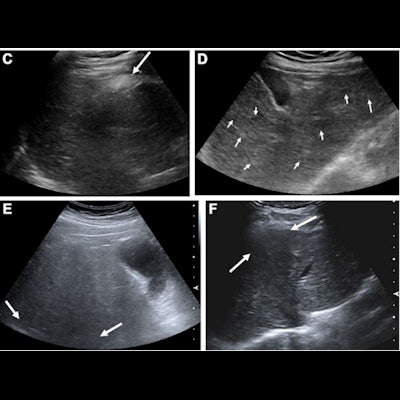
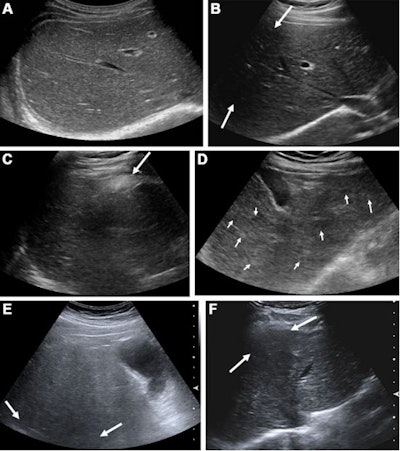 Representative examples of baseline ultrasound images according to the visualization scores and reasons for suboptimal visualization. (A) Visualization A: The liver right lobe was well visualized without any focal lesion with right subcostal scan. (B) Visualization B: With right subcostal scan, the anterior portion of liver right lobe was obscured by shadowing from rib (arrows), and, thus, visualization score B was assigned. (C) Visualization C: With subcostal scan, the liver left lobe and substantial portion of right lobe were not visualized, owing to the shadowing from interposition of the colon (arrow). Because more than half of liver was not clearly visualized, we assigned visualization score C. (D) Suboptimal visualization due to multiple nodules: With subcostal scan, there were multiple subcentimeter size hypo- and hyperechoic nodules (arrows), and, thus, the suboptimal-multiple nodular group was assigned. (E) Suboptimal visualization due to limited penetration: With intercostal scan of liver right lobe, deep portion of liver was obscured (arrows), owing to the limited penetration from fatty liver, and, thus, suboptimal-limited penetration group was assigned. (F) Suboptimal visualization due to limited window: With subcostal scan, the anterior portion of the liver was obscured by shadowing from adjacent rib (arrows), and, thus, suboptimal-limited window was assigned. Images and caption courtesy of RSNA.
Representative examples of baseline ultrasound images according to the visualization scores and reasons for suboptimal visualization. (A) Visualization A: The liver right lobe was well visualized without any focal lesion with right subcostal scan. (B) Visualization B: With right subcostal scan, the anterior portion of liver right lobe was obscured by shadowing from rib (arrows), and, thus, visualization score B was assigned. (C) Visualization C: With subcostal scan, the liver left lobe and substantial portion of right lobe were not visualized, owing to the shadowing from interposition of the colon (arrow). Because more than half of liver was not clearly visualized, we assigned visualization score C. (D) Suboptimal visualization due to multiple nodules: With subcostal scan, there were multiple subcentimeter size hypo- and hyperechoic nodules (arrows), and, thus, the suboptimal-multiple nodular group was assigned. (E) Suboptimal visualization due to limited penetration: With intercostal scan of liver right lobe, deep portion of liver was obscured (arrows), owing to the limited penetration from fatty liver, and, thus, suboptimal-limited penetration group was assigned. (F) Suboptimal visualization due to limited window: With subcostal scan, the anterior portion of the liver was obscured by shadowing from adjacent rib (arrows), and, thus, suboptimal-limited window was assigned. Images and caption courtesy of RSNA.They included data from 2,002 patients with a median age of 54. Of these, 1,192 were men. The researchers placed 972 patients into the optimal group and 1,030 into the suboptimal group. The optimal group consisted of LI-RADS visualization A cases while the suboptimal group included LI-RADS visualization B or C cases.
The team found that during a median follow-up of 75 months, 163 patients developed HCC. Additionally, the suboptimal group had a higher risk of HCC and higher odds of a false-negative rate on ultrasound.
| Comparison between optimal, suboptimal groups | |||
| Optimal | Suboptimal | p-value | |
| Risk of HCC | 0.48% | 2.38% | < 0.001 |
| False-negative rate of ultrasound | 16.7% | 43.9% | 0.04 |
The researchers also reported a hazard ratio of 4.93 for HCC risk in the suboptimal group and an odds ratio of 3.9 for the false-negative rate.
In addition, they found that parenchymal heterogeneity from advanced cirrhosis was the most common cause of suboptimal visualization on ultrasound (n = 489). Other causes included limited window from overlying organ shadow (n = 341) and limited penetration from fatty liver (n = 200).
The study authors suggested that based on their findings, surveillance CT or MRI may be needed for patients with substandard ultrasound. They also called for future research to explore appropriate and cost-effective alternative imaging strategies, as well as links between the visualization score and liver stiffness measured with elastography.
In an accompanying editorial, Richard Barr, MD, from Northeastern Ohio Medical University and Leslie Scoutt, MD, from Yale University suggested that different ultrasound manufacturers may provide different degrees of contrast resolution that affect ultrasound's sensitivity in this area. They also suggested combining ultrasound screening with other clinical and laboratory measures of HCC risk.
"The development of screening guidelines by national and international societies for patients at risk for developing HCC is an extremely important first step in the management of this worldwide medical problem ... ," they wrote. "However, ... another important worldwide trend in healthcare is the recognition of the importance of 'personalized' care within the context of the more structured management template."