The quality of the shear-wave elastography exam matters when creating a prediction model for nonalcoholic fatty liver disease, suggest findings presented April 17 at the American Roentgen Ray Society (ARRS) annual meeting.
In his ARRS Scholars presentation, Dr. Theodore Pierce from Massachusetts General Hospital discussed his team's development of a prediction model for fatty liver disease using imaging biomarkers from elastography. While the model has not achieved high marks in this area, Pierce said the potential is there.
"This is a rapidly advancing field with great excitement in some of the new developments," Pierce said.
Nonalcoholic fatty liver disease affects up to 100 million people in the U.S. Clinical exams, blood-based testing, imaging, and biopsy are used to test for disease. However, Pierce said the field is moving away from invasive methods like biopsy.
Shear-wave elastography is one method used for detecting the disease by measuring tissue stiffness, with diseases tissues having higher stiffness. Pierce pointed out that many biomarkers exist, but none of them are sufficient by themselves.
Pierce and colleagues wanted to better understand shear-wave elastography's use in diagnostic liver imaging. The patients underwent both liver biopsy and elastography. The researchers wanted to incorporate clinical and lab-based biomarkers to see if they could improve elastography's performance in predicting clinically significant fibrosis.
For the model, the team included 1,365 patients with biopsy and elastography pairs. Out of these, 964 had low fibrosis (423 with nonalcoholic fatty liver disease) and 401 had high fibrosis (176 with disease). From there, the team assigned data into training and test sets and explored covariates for inclusion.
Pierce said three covariates that were clinically significant, independent predictors of liver fibrosis were selected for inclusion in the model. These included the presence or absence of diabetes (odds ratio [OR], 2.09), platelet count (OR, 0.996), and liver stiffness measured on elastography (OR, 1.078).
Using these, the multiparametric model achieved an area under the curve (AUC) of 0.723 in the training set and 0.738 in the validation set. These surpassed comparative models using only imaging, though these were "marginal" across the board. Additionally, when using a high sensitivity threshold, specificity was low at 44.6%. On a high specificity threshold, sensitivity was 30.4%.
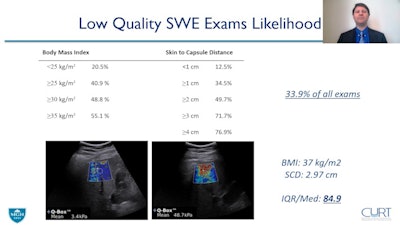 Dr. Theodore Pierce from Massachusetts General Hospital describes a predictive model using shear-wave elastography for nonalcoholic fatty liver disease. He and colleagues found that BMI and skin-to-capsule distance impacts elastography exam quality, which could lead to poor disease mapping. Pierce et al's research was funded in part by an ARRS scholarship. Image courtesy of the ARRS.
Dr. Theodore Pierce from Massachusetts General Hospital describes a predictive model using shear-wave elastography for nonalcoholic fatty liver disease. He and colleagues found that BMI and skin-to-capsule distance impacts elastography exam quality, which could lead to poor disease mapping. Pierce et al's research was funded in part by an ARRS scholarship. Image courtesy of the ARRS.Pierce said one part that the team did not take into account was the quality of elastography exams. After eliminating low-quality images from the multiparametric model, the AUC improved to 0.758.
On subgroup analysis, the fatty liver disease cohort had an AUC of 0.714 on the model, but this improved to 0.747 after excluding low-quality images.
When comparing receiver operator characteristic (ROC) curves for low- and high-quality elastography exams, the model had a ROC curve of 0.791 for the high-quality group and 0.602 for the low-quality group.
"There's a remarkable difference in looking at the diagnostic performance of elastography alone with filtering out the low-quality exams," Pierce said.
So, what caused these low-quality exams? Pierce noted that body mass index (BMI) and skin-to-capsule distance are known factors of poor disease mapping. For the study, the team reported that these were significantly associated with low-quality exams, with AUCs of 0.699 for BMI and 0.744 for skin-to-capsule distance.
Pierce said that these two factors are important, because patients with high BMIs or higher skin-to-capsule distances may not be eligible for shear-wave elastography. For these patients, blood-based testing or MRI elastography may be the better choices.
Pierce said that these results reflect a real-world implementation of shear-wave elastography in a multiparametric model. While there is room for improvement, he said there is hope in the form of ongoing efforts to improve hardware and signal processing, as well as increase acoustic output, among other areas.
"Because of this enormous public health crisis and the growing rates of fatty liver disease associated with the obesity epidemic, it's critical that we develop tools to identify liver fat, liver fibrosis, and inflammation to identify at-risk patients," he said.