Quantitative angiogenesis-based ultrasound biomarkers can differentiate between radial scar lesions and breast cancer, suggest findings published October 14 in The Breast.
A team led by Azra Alizad, MD, from the Mayo Clinic in Rochester, MN, reported differences in microvessel structure between radial scars and invasive ductal carcinoma. They also identified several biomarkers tied to differences between these two imaging findings.
“These results suggest that malignant tumors, such as invasive ductal carcinoma, possess more complex, irregular, and denser vascular networks than radial scarring,” Alizad and colleagues wrote.
While radial scars are benign, they share some features with invasive ductal carcinoma. These include spiculated margins, posterior acoustic shadowing, and architectural distortion. Mammography, MRI, and ultrasound may not be able to provide a definitive diagnosis of radial scars, leading to biopsy.
The development of new blood vessels in tumors -- angiogenesis -- may play a role in cancer diagnosis. Prior research suggests that blood vessels in malignant tumors show more heterogeneity and differ from vessels in normal tissues or benign tumors.
Alizad and colleagues developed a contrast-free ultrasound-based technology called quantitative high-definition microvasculature imaging (qHDMI). They noted that this approach can image submillimeter vessels as small as 150 μm and quantify tumor microvessel morphology.
The team studied the effectiveness of quantitative biomarkers from qHDMI for differentiating between radial scars and invasive ductal carcinoma. The study included 64 breast lesions from 62 women, with breast pathology serving as the gold standard.
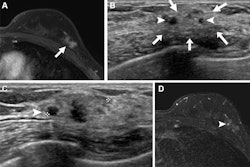
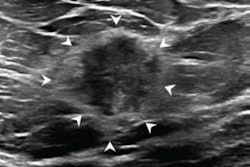
 Examples of an 18 mm radial scar (top row) and a 15 mm invasive ductal carcinoma (bottom row) breast lesions. (a,d) show clinical B-mode images, (b,e) depict B-mode images in plane wave imaging mode, and (c,f) illustrate qHDMI generated microvasculature images. Tables to the right of the images indicate qHDMI biomarker values. The blue and green dashed curves indicate the segmented lesion boundaries, before and after 2mm dilation, respectively. Images are republished under a Creative Commons license (CC BY-NC-ND 4.0).
Examples of an 18 mm radial scar (top row) and a 15 mm invasive ductal carcinoma (bottom row) breast lesions. (a,d) show clinical B-mode images, (b,e) depict B-mode images in plane wave imaging mode, and (c,f) illustrate qHDMI generated microvasculature images. Tables to the right of the images indicate qHDMI biomarker values. The blue and green dashed curves indicate the segmented lesion boundaries, before and after 2mm dilation, respectively. Images are republished under a Creative Commons license (CC BY-NC-ND 4.0).
Of the total lesions, 17 were pathologically confirmed as radial scarring and 47 as breast cancer. The team reported that the malignant lesions showed denser, thicker, and more complex microvessels.
The team also reported five biomarkers from qHDMI that showed statistically significant distribution differences, even when adjusted for multiple testing. These biomarkers also achieved moderate area under the curve (AUC) values.
Biomarkers tied to distribution differences between radial scar, invasive ductal carcinoma | |||
Biomarker | AUC | p-value (unadjusted) | p-value (adjusted) |
Vessel density | 0.7 | 0.016 | 0.029 |
Number of vessel segments | 0.73 | 0.005 | 0.029 |
Number of branch points | 0.71 | 0.01 | 0.029 |
Maximum diameter | 0.7 | 0.014 | 0.029 |
Microvessel fractal dimension | 0.7 | 0.018 | 0.029 |
The study authors highlighted that qHDMI’s processing framework can be implemented on data gathered “from any ultrasound system capable of acquiring high-frame-rate ultrasound data.”
“The image processing pipeline can potentially be implemented in other programming languages,” they added. “Moreover, the objective nature of data processing in the framework, removes operator dependency and variability.”
The authors also called for multi-institutional studies to further investigate the efficacy of these biomarkers in larger patient populations, suggesting that moving from 2D to 3D qHDMI could further improve upon their findings.
Read the full study here.