Botox injections combined with an anti-nausea patch may help advanced metastatic castration-resistant prostate cancer (mCRPC) patients avoid severe dry mouth and continue their radioligand therapy, suggested early research presented June 24 at the 2025 Society of Nuclear Medicine and Molecular Imaging (SNMMI) annual meeting.
Salivary gland toxicity is a known side effect of some prostate-specific membrane antigen (PSMA)-targeted radioligand therapy (RLT) -- especially alpha-emitting actinium-225 (Ac-225) -- that can lead to debilitating dry mouth syndrome, or xerostomia, according to a group led by Jingjing Zhang, MD, PhD, of the Theranostics Centre of Excellence in the Yong Loo Lin School of Medicine at the National University of Singapore.
However, the combination of botulinum toxin (BTX) Type A (IncoA) and the nausea patch (scopolamine) may offer a dual-protective approach and both, having established safety profiles, could be immediately applied in experienced centers offering PSMA radioligand therapy, Zhang and colleagues wrote.
To explore the impact of the dual approach, the group conducted a preclinical, early-stage radiopharmaceutical oncology study that included 14 patients undergoing one to two cycles of tandem PSMA-targeted radioligand therapy, lutetium-177 (Lu-177) at 5.05 ± 1.09 GBq and Ac-225 at 6.87 ± 3.14 MBq per cycle.
Each patient received 16 BTX treatments consisting of 115 to 250 units of ultrasound-guided BTX IncoA injections in their parotid glands, and between 70 to 80 units in their submandibular glands on opposite sides of the body, three to four weeks prior to their combined Ac-225 and Lu-177 PSMA therapy. Four patients were treated with BTX alone, while the others received a combination of BTX plus the scopolamine patch.
Three days before treatment, the nausea patches were applied behind the ears, where they remained until two hours after the treatment.
The patients also underwent pre-therapy PSMA PET/CT to confirm tumor and salivary gland uptake and SPECT/CT post-therapy for restaging, according to the team.
The researchers found that BTX-treated parotid glands showed a mean 30% reduction (range 19% to 47%) in PSMA uptake (p < 0.001) compared to the opposite parotid gland. They also reported a mean 17% reduction (range 10-51%) in PSMA uptake in injected submandibular glands (p = 0.004) compared to the opposite submandibular glands.
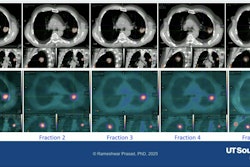
Post-injection SPECT/CT images revealed a marked reduction in PSMA radioligand uptake in the BTX-treated glands, with parotid gland uptake ratio shifting from 0.93 to 1.15 and submandibular gland ratio from 1.39 to 2.14, confirming targeted protection, the investigators noted.
 In a patient, pretreatment PET/CT demonstrated comparable tracer uptake. Postinjection SPECT/CT images revealed a marked reduction in PSMA radioligand uptake.SNMMI
In a patient, pretreatment PET/CT demonstrated comparable tracer uptake. Postinjection SPECT/CT images revealed a marked reduction in PSMA radioligand uptake.SNMMI
Patients who received BTX without scopolamine showed no significant difference in the uptake between injected and noninjected salivary glands, they reported, adding that injections generally were well tolerated and, importantly, no patient discontinued combination PSMA therapy due to dry mouth.
One injection-related local hematoma occurred in a patient with thrombocytopenia, the team reported. Also, scopolamine-induced moderate dry mouth occurred but lasted 72 hours.
“This study offers a promising therapeutic strategy for reducing radiation-induced salivary gland toxicity without compromising PSMA tumor uptake,” Zhang said. “The significance of this work lies in its direct patient benefit and its potential to expand the therapeutic utility of PSMA radiopharmaceutical therapy, particularly with alpha-emitting radionuclides like 225Ac.”
The investigators concluded that the combined approach may enhance patient quality of life following PSMA radioligand therapy, particularly with alpha-emitting radionuclides, although further studies with larger patient cohorts and longer follow-up periods are warranted.