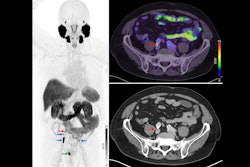
Prostate-specific membrane antigen (PSMA) PET imaging can improve survival outcomes for men undergoing salvage radiotherapy after prostatectomy, according to a study published October 2 in JAMA Oncology.
The finding is from a phase II trial that met its primary endpoint, with a phase III study planned to confirm the results, noted first author Colin Belliveau, MD, of the University of Montreal in Quebec, Canada, and colleagues.
“Given its impact, PSMA-PET should be performed to guide [salvage radiotherapy] for patients presenting with a [biochemical recurrence] after [radical prostatectomy]. A subsequent phase III randomized clinical trial has completed accrual and will shed further light on those patients who benefit most,” the group wrote.
After radical prostatectomy, some patients will experience a biochemical recurrence of prostate cancer based on rising prostate-specific antigen (PSA) levels. Even though salvage radiotherapy (SRT) has been shown to improve outcomes in these cases, more than a quarter of patients still have another recurrence, the authors explained.
Given the high sensitivity and specificity of PSMA-PET for detecting prostate cancer, the researchers hypothesized that it could improve survival outcomes for patients if used prior to SRT compared to SRT without PSMA-PET guidance.
The study randomized 128 patients with biochemical recurrence after surgery to receive either standard-of-care SRT (n = 64) or PSMA PET-guided SRT (n = 64). Most patients in each group also received androgen deprivation therapy. The primary end point was failure-free survival (FFS), defined as the first occurrence of biochemical progression (PSA > 0.2 ng/mL), clinical progression, initiation of next-line therapy, or death.
The median PSA at enrollment for patients was 0.3 (0.1-3) ng/mL. Out of the 64 patients in the experimental arm, 33 (52%) had positive PSMA-PET scans and received intensified SRT. At a median follow-up of 37 months, these patients had an improved FFS (hazard ratio [HR], 0.5; p = 0.04) compared with the control group, according to the results.
The greatest benefit was seen in a subgroup with PSA levels of 0.3 ng/mL or more (HR, 0.17; p = 0.01), and fewer next-line treatment events occurred in the patients who underwent imaging versus those who did not (4 vs. 12; p = 0.04). Finally, there were no significant differences in toxic effects or quality of life between the groups, the researchers reported.
“This is the first randomized clinical trial demonstrating an isotoxic improvement in prostate cancer control outcomes with intensification of SRT informed by PSMA-PET,” the group wrote.
In an accompanying editorial, Sophia Kamran, MD, of Massachusetts General Hospital in Boston, and James Yu, MD, and Nirav Kapadia, MD, of Dartmouth College in Lebanon, New Hampshire, noted that findings raise several additional questions.
“First, how do we incorporate other prognostic tools, including genomic and digital pathology signatures that also provide guidance regarding therapy (de)escalation?” the authors wrote.
Other questions include what to do with patients with a PSA level of less than 0.3 ng/mL and what the role could be for prolonged ADT or androgen receptor pathway inhibitors among patients with PET-detected disease.
"We congratulate the authors for this study. Sometimes, the best studies simultaneously resolve and raise new questions," Kamran, Yu, and Kapadia concluded.
The full study is available here.