PACS has proven its power to make healthcare organizations more competitive in many ways, from radiological productivity and diagnostic effectiveness to the satisfaction of referring physicians and their patients. But will your unique mix of PACS technology and workflow deliver merely adequate results, or outstanding performance? How can you extract from PACS the greatest clinical benefit and highest return on investment?
Each component of the PACS environment presents opportunities to optimize. Examples include image retrieval, transport and delivery, workflow design, management, and training. Workflow -- the human element -- is an integral part of the PACS environment.
In fact, it’s impossible to separate digital imaging infrastructure from the patients, clinicians and other personnel who must rely on PACS. Therefore, only a holistic approach can yield optimal results. Achieving them means looking at PACS technologies, business processes, and human factors as an interactive, interdependent whole.
Some healthcare organizations are laying groundwork for their initial PACS deployment, while early adopters may be planning to refresh their technology. In either case, these optimization rules apply:
- Align PACS investments with strategic goals. Update PACS planning to keep abreast of evolving strategies, such as shifts in the organization’s competitive position or its treatment emphasis.
- Distinguish between needs and wants. Identify the factors that truly drive your need for change. Prioritize.
- Set measurable objectives and perform before-and-after measurements. One healthcare chief information officer (CIO) said this practice was key to obtaining, and retaining, budget approvals for PACS as deployment unfolded.
- Recognize that a PACS deployment is a continuing process. Whether it’s for now or later, accept refreshment of technology as a necessary cycle.
- Rely on open architecture and standards. This allows for change with the greatest flexibility and scalability, while avoiding excessive cost.
- Implement RIS before PACS. A hospital information system (HIS) typically lacks data structures that many experts view as crucial to supporting PACS and radiology workflow. By contrast, these structures are built into radiology information systems (RIS). Without RIS, the benefits of PACS will be greatly diminished.
- Perform a detailed business analysis. From an economic feasibility standpoint, it will determine what you should do, when to do it, and what results you must achieve to be deemed successful.
In addition, sensible practices include adhering to DICOM standards, avoiding proprietary databases, and building future expansion into the storage solution. An often overlooked practice, workflow analysis and training should be integrated into every aspect of PACS. Workflow modifications and training reduce the pain and risk of changes while improving outcomes and financial returns.
Goals and expectations
Digital image management can deliver efficiencies that enable the organization to increase the annual volume of studies performed for departments ranging from orthopedics to cardiology and oncology. PACS technology and workflow can satisfy physicians’ demand for quick, convenient access to images, and shorten patient wait times in radiology.
Planning PACS may also offer opportunities for consolidating mini-PACS networks serving individual departments -- or avoiding the need to use them in the first place. A single integrated PACS solution is easier to manage and maintain. Goals such as these underscore the need to closely align PACS planning with the organization’s strategies and competitive situation.
Considering these realities, how do you optimize PACS design and deployment to align with goals and support organizational strategies? Examples may be drawn from image retrieval, transport and delivery, workflow improvements, and technology optimizations such as image display, archiving and distribution.
Retrieval
At times, optimizing PACS may be as simple as tuning various hardware and software features that may not be ideally configured or even turned on. Image retrieval offers a case in point. The PACS can anticipate which images a physician may request from storage and "pre-fetch" them, effectively speeding retrieval.
The pre-fetch function may be tuned to optimize performance, for example by pre-fetching historical images of a patient’s specific body part when the day’s radiology exam schedule calls for a new study of that part. Such tuning can reduce network traffic, thus improving performance for all users, by eliminating pre-fetch of images that are less likely to be relevant.
Transport
Institutions can improve network performance similarly by matching users to the quality of images requested over the network. Data traffic rises dramatically with the level of detail in images being transported. For example, a fully detailed, 14 x 17-inch computed radiography image generates approximately 12 megabytes of data over the network. Mathematically compressing the image at 32:1 causes some visual detail to be lost, but the resulting image would occupy only 384 kilobytes and, allowing for fixed network overhead, could typically ease network loading by 85 %.
While not suitable for diagnosis, a highly compressed image could serve some needs quite well. Non-diagnostic clinical users such as PAs might normally use an intermediate level of compression. By matching image quality defaults to user types, network performance can be improved significantly.
Delivery
Radiologists’ efficiency and effectiveness are enhanced -- and potential diagnostic error reduced -- when hanging protocols are tailored precisely to individual needs and preferences. A radiologist should be able to specify, "When I look at chest x-rays, I want the new study on the left and the old study on the right. Further, I want the PA version up first, then the lateral."
PACS networks should present these defaults whenever this radiologist logs onto a diagnostic workstation, with each radiologist able to specify his own default preferences. Getting the hanging protocols right may require more than simply inserting a set of preferences into PACS software.
It may also demand a change in radiology technicians’ workflow. Technologists acquiring the study may have to submit images to the PACS network in the proper sequence for storage, so that they come up for viewing in the same sequence in which they were acquired or stored.
There are also other cases in which optimizing the end-user experience may require also changing upstream events, i.e. workflow.
Workflow
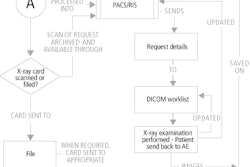
Analyzing and modifying workflow can produce many positive impacts. One New England facility we work with experienced workflow challenges faced by many healthcare organizations: radiologic technologists using PACS still spent more than half their time on administrative tasks such as managing requisitions from referring departments -- for instance, phoning a physician to clarify an order and then modifying the order in the RIS.
By hiring administrative aides to handle such tasks and by giving order-entry classes to personnel in referring departments, tech productivity was essentially doubled. Hospitals must look for opportunities like this to streamline traditional workflow previously designed around film.
At the New England facility mentioned above, clinics commonly sent patients to radiology and held them there until a radiologist viewed the images. This linear process made sense in a film environment. Film would accompany the patient back to the orthopedist, who awaited their turn to read the film.
PACS accelerated this facility’s clinical workflow and eliminated the need to keep patients waiting in the radiology department. Because PACS workstations were deployed to referring physician areas, an orthopedist could now view images at the same time as the radiologist.
Workflow also offers opportunities for reducing clerical errors that slow processes, sap productivity, and raise costs. Information is sometimes manually re-keyed when it crosses a boundary, such as between the HIS, RIS, PACS, and modalities. Automating data propagation across such boundaries eliminates numerous errors.
In some cases, errors continued to hamper operations even after radiology workflow was optimized. These errors were traced back to personnel in referring departments who were making errors in ordering studies. Retraining these FTEs, and in some cases modifying their workflow, eliminated the problem.
Technology
Whether planning PACS for the first time or considering a technology upgrade, deployment decisions and ultimate results may be affected by recent trends. For example, Web-based PACS has become common. Two other advances worth considering are flat-panel displays and RAIN (redundant array of independent nodes) data storage.
Display. Flat panels have become a better long-term solution than CRTs. Today’s flat panels offer more brightness and sharper focus than CRTs, delivering a superior image with less eyestrain.
Hospitals regain space currently monopolized by CRTs, especially the footprints required for large, multi-headed diagnostic displays. And flat panels can mount on walls or ride on mobile stands, providing unprecedented flexibility.
While their purchase cost may be substantially higher, flat panels are inherently more reliable and provide a longer lifespan, driving down total cost of ownership well below that of CRTs. This long-term cost advantage suggests that hospitals should consider replacing traditional desktop monitors as part of general refreshing of PC technology. This type of program may be dovetailed with PACS deployment to provide more effective image display.
Archiving. The per-terabyte cost of data storage media continues to fall, now making spinning disk the archive medium of choice for storing all but the oldest digital images. Some providers with older PACS are replacing off-line optical storage media with disk storage.
Managing and preserving terabytes of data also is becoming easier and more reliable with the advent of RAIN technology. RAIN is essentially a RAID of RAIDs (redundant arrays of independent disks). It offers sophisticated error checking, redundancy and failover, so problems with a disk or even multiple disk drives won't cause data loss.
Also, today’s RAIN-based archives are fast. A data request that took 30 to 60 seconds using older technology now takes 10 seconds with RAIN.
Conclusion
Any given PACS solution can deliver results ranging from adequate to exemplary, depending on how its infrastructure and workflow are implemented. The results affect the organization’s competitiveness in several ways, including efficiency, clinical effectiveness, and physician and patient satisfaction.
Numerous factors affect PACS optimization, including understanding the PACS life cycle, adhering to standards, addressing workflow issues, assessing recent technology trends and fine-tuning image handling including retrieval, transport and delivery. By optimizing PACS, hospitals and multi-facility systems can improve clinical practice, increase return on investment and compete more effectively in a challenging healthcare environment.
By John NormanAuntMinnie.com contributing writer
February 2, 2004
John Norman is business unit executive for digital solutions unit of Xtria, a Dallas-based company providing digital imaging management, integration, and implementation solutions and services.
Related Reading
Keeping your eye on the PACS ball, September 30, 2003
Smoothing the transition to filmless, June 16, 2003
Copyright © 2004 AuntMinnie.com