Implementing PACS requires careful consideration of how to handle the radiology ordering process. Giving up a card-based ordering system in favor of electronic ordering offers compelling benefits as well as some challenging drawbacks.
Keeping the card?
Maintaining the card system allows for maintaining the current process of ordering an x-ray study, with its associated higher quality of clinical details. The disadvantage, however, is a non-paperless solution.
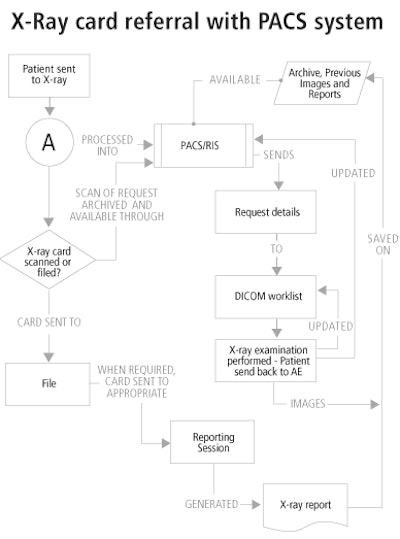
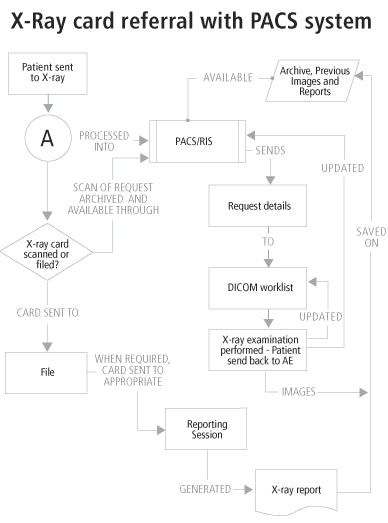
There are two workflow options with the card, shown in flowcharts A and B below. The manual input of patient details into the radiology information system (RIS) is outlined in flowchart A.
- The card can be canned and be saved as a JPEG image that can be "attached" to that patient’s x-ray images, with instant availability upon the click of a ‘request card’ icon. This would then open up in a new window, which would be sized accordingly to enable simultaneous viewing of both the image and request card.
- In the second workflow option for the card system (flowchart B), the card is filed and put away after the examination. However, a major problem here occurs when the radiologist goes to report, as the card must be physically present at the workstation for the reporting process. It may be difficult to predict which radiologist would report on each examination and at which workstation. A radiologist may also wish to do some reading at any moment during the day on any given patient if a relatively common reason arises. With this approach, the radiologist would have to go and look for the card.
Once the patient arrives at the x-ray unit with the referral card, medical information is extracted from it in the normal way (flowchart A) and the patient is processed onto the DICOM worklist for examination. The card now has to be scanned and attached electronically to those patients’ details, and can then be discarded.
The advantage here is that the request details would instantly be available to the radiologist during reporting, wherever and whenever they wanted. However, patient details still need to be entered onto the RIS/PACS in the normal way in addition to the scanning process, adding more work. As this may have already been performed on a hospital information system (HIS) in Accident and Emergency (AE) departments, outpatient (OP) units, or the ward, this step may seem unnecessary.
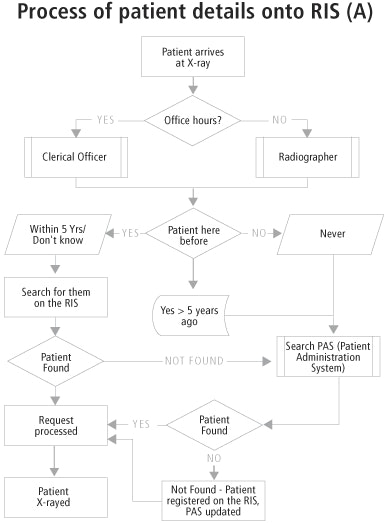
As seen in flowchart A, the process of entering patient details into the RIS has to be incorporated into the card referral flowchart, making the whole process considerably large and more complicated.
Other problems occur with the card itself. Extra staff are needed to file away and extract up to 60,000 cards (or whatever the case may be) a year. How long do we keep them for? Do we have the space? How do we link up multiple referrals together? The extremely laborious nature of this job would be unlikely to attract clerical staff to radiology.
Paperless environment
The alternative, of course, is an electronic online ordering referral system. With this approach, the clerical work is, in essence, moved to the point of referral. With AE, OP’s, and the wards having their own clerical staff, this may not be a problem.
The clerical staff input/update the patient details on the HIS, which would then have an electronic ordering facility should the treating physician require it. Upon entering the clinical details and the examination requested, the order could be sent electronically to the RIS, which could immediately update the system and the DICOM worklist.
The patient is now ready to enter the x-ray room, with no need for clerical staff to process x-ray request cards. Radiographers don’t have to process request cards when on-call, with patients being taken straight from the DICOM worklist. The result is a quicker examination.
Because the system is not maintained independently from the images, there’s no possibility of separation. Patient details are entered onto the RIS/HIS at the patient’s point of entry into the hospital, so there’s no need for separate entries in different departments.
Even when the patient has requests for different examinations in different departments, they must be entered into the system only once. There is no need to write out a x-ray request, a CT request, a blood work request, etc., since these could be ordered with a few mouse clicks once the patient has been entered on the system.
With patients immediately being sent to the DICOM worklist, this information can be made to show up immediately on the on-call radiographer’s personal digital assistant (PDA). As a result, the radiographer doesn’t need to be called, and the patient could walk straight into the x-ray room for examination.
The electronic report could be sent back via the same channel as the electronic ordering system. With the use of digital radiography and integration of wireless technology, patients could experience dramatic reductions in time spent in the radiology department.
With the inherent need for a seamlessly integrated PACS/RIS solution, an electronic ordering system could bring together a common goal for both vendors and may lead to better overall integration of the PACS and the RIS. This could also be considered a drawback, however.
If the HIS system goes down, however, there is no way to order an x-ray without going back to a card system. With a card system, patients could still be entered on the RIS/PACS network if the HIS goes down, with data being matched up at a later date when the system is restored.
Drawbacks
Electronic ordering brings its own challenges. Clerical input of patient data normally performed in the x-ray department is now handled at the source of the request, creating additional responsibilities for the AE and OP units. In our experience in the x-ray department, it’s quite difficult to get non-clerical staff to start entering patient details.
If patient details are already being entered electronically in AE, however, this information alone can be used to supplement an electronic order. The only subsequent details needed are the examination and clinical details.
Conversion to an electronic ordering system also brings the potential for loss of clinical details. For radiologists this is a major issue. In our unit, the general feeling is that very little attention would be paid to clinical details if a request were made electronically. It only takes a few seconds to jot down a few handwritten notes that give clinical details about why the examination is to take place and what is the particular area of interest.
In contrast, a request typed into a computer would likely take a lot longer for most people. While a drop-down menu facility for pre-defined clinical details is an option, there is still potential for misuse. The easiest accessible drop-down selection could be used continuously or perhaps even set to a default setting.
It’s also a challenge to confirm the validity of the imaging request. Currently, only doctors are allowed to request x-rays. If there is a query on the request card, you just follow up the signature of the requestor.
With an electronic ordering system, it’s difficult to completely ascertain who requested the exam. Dr. X could have left his computer workstation in a hurry in the middle of AE. Then somebody else might come along, someone who is not in a position to order an x-ray, and start ordering them.
If there were to be a problem with patients being overexposed, who would get the blame? There would be no proof that a certain person ordered an exam. It could possibly have legal implications. A strict sign-on system could be enforced, whereby whoever is logged on to the system at the time of the request is responsible for that request. However, doctors don’t want to have to sign in every time they are to order an x-ray.
A swipe card system is used at some institutions, in which each doctor is issued with a swipe card that has to be slotted into the workstation keyboard in order for a request to take place. But with most doctors that request x-rays changing every six months, this could be difficult to enforce and keep track of swipe cards.
It seems that whatever solution is chosen, there will always be the potential for misuse.
Solutions for GP requests
Accommodating general practitioner (GP) imaging requests may not be as straightforward as in-house ordering. With an electronic ordering system, GPs would need access to the RIS network -- not a viable solution.
Most GPs, who may be in remote locations, will probably prefer to stick to their current method of request, which basically entails filling out an x-ray request form in a couple of minutes and handing to the patient. Patients make the appointment on their own, and then proceed to our institution to have the exams performed.
Anybody who is not used to computers (or even those who are) may not want to start doing this process over the Internet. It’s difficult to validate the requestor and to determine whether or not somebody hasn’t hacked into his or her ordering facility.
With GP’s accounting for less than 5% of our total patient numbers, it might not be too difficult to make an exception and have the manual input of requests cards available to them.
Conclusion
An electronic ordering system can be a viable solution for AE referrals, and perhaps, for outpatient clinics and the wards. While this type of system makes the radiology examination a much simpler process, there are also substantial challenges to overcome.
By Pauric GreenanAuntMinnie.com contributing writer
January 6, 2004
Pauric Greenan is PACS project coordinator at Midlands Regional Hospital Tullamore in Ireland.
Related Reading
RIS/PACS integration brings productivity, efficiency gains, July 22, 2003
Online scheduling improves satisfaction, July 3, 2003
Smoothing the transition to filmless, June 16, 2003
Primary care reminders reduce x-ray requests, September 27, 2002
The parlous state of UK radiology, September 24, 2002
Copyright © 2004 AuntMinnie.com