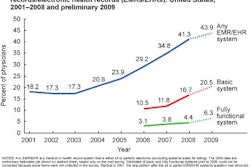
On July 13, U.S. physicians and hospitals received their marching orders on how to receive federal incentive payments for adopting electronic medical records. But the question remains: What does this mean for radiology?
The rules, which were issued by the U.S. Centers for Medicare and Medicaid Services (CMS) and the Office of the National Coordinator (ONC) for Health Information Technology, clarify provisions of the American Recovery and Reinvestment Act of 2009 and the Health Information Technology for Economic and Clinical Health (HITECH) Act that require healthcare providers to show they are "meaningful users" of electronic health record systems over a specific timeline before qualifying for funding.
Under the laws, the federal government will pay eligible individual physicians up to $44,000 under Medicare and $63,750 under Medicaid. Hospitals have the potential to receive millions of dollars in payments. The cost to the federal government will depend on the number of healthcare providers who qualify, but it is estimated at $9.7 billion to $27 billion, according to CMS.
The deal is further sweetened by enabling physicians to report only 90 days of data in their first year of participation to receive payment. Also, payments will be made in a lump sum each year, as soon as physicians prove they are meeting the meaningful use requirements.
What do these final rules mean to radiologists, the digital pioneers of IT adoption among medical specialties? What has changed from the proposed rules issued in January 2010? Do radiologists benefit from any of the changes?
No easy answers
Answering these questions isn't easy, as there are more than 1,000 pages of regulations and commentary to read. However, the American College of Radiology (ACR) in Reston, VA, has published a succinct explanation and analysis of the rules on its website as they pertain to radiologists. AuntMinnie.com talked with Michael Peters, ACR assistant director, regulatory and legislative portfolio.
In March, the ACR; the American Board of Radiology (ABR) of Tucson, AZ; the RSNA of Oak Brook, IL; and the Society for Imaging Informatics in Medicine (SIIM) of Leesburg, VA, jointly commented about both proposed rules as they related to radiology. The societies' recommendations were among the more than 2,000 received by CMS and ONC.
"The most important and most positive change is the flexibility added to the meaningful rules," Peters said. "Exclusion criteria were added for many core and elective discretionary measures, and flexibility of selection of discretionary 'menu set' measures was also added. Collectively, these improvements allow for more variability in physicians' scopes of practice, whereas in the previous proposed rule, all physicians needed to fully satisfy all 25 measures without any exceptions."
Eligibility criteria have also been redefined, so that the majority of radiologists now qualify to participate in the program, whether or not they are hospital employees or exclusively affiliated with a private practice or teleradiology service. Any healthcare professional who provides more than 10% of professional services outside inpatient and/or emergency room settings can be eligible. CMS estimates that 86% of all Medicare participating physicians will now be eligible under the new criteria.
Requirements to achieve 'meaningful use'
With the goal of enabling physicians and hospitals to realistically succeed in achieving the first stage of implementation requirements, CMS has reduced the requirements from 25 to 20 for eligible medical practices and from 23 to 19 for hospitals. Requirements have been divided into a group of 15 core requirements and 10 discretionary requirements, of which five must be met.
For many of these requirements, levels of attaining electronic utilization have been reduced, some significantly. Previously included criteria that could have been problematic, such as capturing health insurance information as structured data, have been eliminated.
The core/discretionary two-track approach is designed to ensure that the most basic elements of meaningful use will be met by all providers qualifying for incentive payments, while at the same time allowing latitude in other areas to reflect the providers' needs and the methods by which they choose to achieve meaningful use, according to CMS.
But some of the requirements are not applicable to the practice of radiology -- which is where the exclusions step in. Exclusions are also counted as satisfying the requirements of a measure, which will benefit radiologists.
Requirements for computerized physician order entry (CPOE) of prescriptions, laboratory tests, and diagnostic imaging exams are not applicable to the radiology specialty. As long as radiologists write fewer than 100 prescriptions during the reporting period, they can be exempt from satisfying two of the core electronic prescription requirements: using CPOE for medication orders and having the ability to generate and transmit permissible prescriptions electronically. Under the CMS definition, a "prescription requires a specific physician-to-pharmacist interaction and authorization," so contrast media is considered a "supply" rather than a prescription.
Radiologists have the choice of installing individual certified electronic health record (EHR) modules, which in combination can meet all of ONC's certification criteria, or of utilizing a comprehensive certified EHR system, which by itself meets all of ONC's certification criteria. If the EHR module approach is selected, a certified radiology healthcare IT product could potentially include a list of all the medications being taken by a patient, confirmation that drug-drug and drug-allergy interactions have been checked, and a field for known medication allergies of a patient (three core requirements).
Patient demographic information including gender, race, ethnicity, date of birth, and preferred language needs to be recorded in structured data format for at least 50% of a physician's patients. Diagnoses or an indication that no clinical problems have been identified for the patient need to be captured for 80% of the patients (two core requirements).
Medical records must also include other patient information including height, weight, blood pressure, body mass index, and -- for children ages 2 to 20 years -- growth charts, for at least half of the patients. However, if this information has no relevance to a scope of practice, an exclusion may be claimed. This exclusion option is specifically applicable to teleradiology service providers.
However, no radiologist who interprets exams of patients older than age 13 is exempt from the requirement of recording a patient's smoking status. This information, like other patient demographic information, may be provided by the referring physician if not collected by radiology department or imaging center support staff.
Participating radiologists will need to implement and track at least one clinical decision-support rule. Radiologists can define any clinical decision-support rule to track to meet this requirement.
Participating radiologists would also need to test the exchange of "key clinical information" with other healthcare providers. The final rule gives physicians the authority to define which clinical information is considered "key."
Proof of maintaining secure data by conducting security risk analyses and implementing security updates is required. These are undisputed common-sense steps for any radiologist using digital technology.
As with core requirements, exclusions can help radiologists accelerate the process of meeting five of 10 discretionary requirements. Exclusions that radiologists most likely would claim include submitting electronic data to immunization registries and ordering clinical laboratory tests.
Of the remaining three requirements, several items may be less challenging to fulfill. These include sending reminders to patients who need follow-up examinations, such as mammograms; providing at least 10% of patients with timely electronic access to their health information, such as radiology reports; providing patient-specific educational resources to at least 10% of the patients, as determined by the radiologist; and providing summary of care records, which could be paper-based, by DICOM CD/DVD, or by direct electronic transfer, to patients seeing another physician.
CPOE for imaging
Considering the ACR's support for the use of CPOE with integrated clinical decision support based on appropriateness criteria, Peters said that CMS' exclusive focus on medication orders during the first stage of implementation was disappointing.
"From a quality and cost-savings perspective, ordered services such as diagnostic imaging should have been included in the CPOE meaningful use measure for stage 1," Peters said. "This is the primary way to curb inappropriate utilization or overutilization by referring physicians. The national coordinator for health information technology, Dr. David Blumenthal, has himself spoken publicly about the clinical utility and cost-effectiveness of appropriateness criteria guidelines during the radiology services ordering process."
But there is a way that CPOE use might extend beyond ordering prescription drugs in stages 1 or 2 of meaningful use, Peters noted.
"The ONC rules for certification criteria, standards, and implementation specifications are not in sync with CMS' final meaningful use rules in a number of ways," he said. "To be certified, the products themselves will have to include the ability to electronically order diagnostic imaging exams, laboratory tests, and medication orders. With the radiology order-entry capability in place, referring physicians might need to use CPOE for radiology exams in the future."
"I think that successful participation by eligible radiologists will require a certain degree of change and ingenuity, but the most challenging component will probably be the technology piece," Peters concluded. "It will be interesting to see industry develop clinically useful, cost-effective, and certified solutions that will facilitate radiology's participation in the program."
The ACR summary of final stage 1 meaningful use rules may be accessed by clicking here.
By Cynthia E. Keen
AuntMinnie.com staff writer
July 29, 2010
Related Reading
CMS issues final 'meaningful use' EHR rules, July 13, 2010
ONC rules on EHR certification, June 18, 2010
Medical societies challenge CMS proposal for EHR adoption, May 10, 2010
Radiology societies comment on HIT stimulus, March 17, 2010
Don't ignore imaging when planning healthcare IT stimulus goals, March 9, 2010
Copyright © 2010 AuntMinnie.com