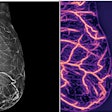
Surveillance imaging of women with ductal carcinoma in situ (DCIS) that has progressed to invasive disease visualizes particular imaging features, according to research shared at the Society of Breast Imaging (SBI) meeting in National Harbor, MD.
Dr. Derek Nguyen from Duke University in Durham, NC, presented study findings that showed that when DCIS develops into invasive ductal carcinoma, it most commonly appears as new calcifications and new masses.
"This is a descriptive study that helps flesh out more details on what patient populations are more at risk and how we [radiologists] can detect disease progression as early as possible," Nguyen told AuntMinnie.com.
DCIS cases can be tricky. As many do not progress into invasive cancers or take years to do so, concerns persist about overdiagnosis. Along with that, radiologists are challenged to determine which women who have DCIS are more at risk for disease progression than others. Surveillance imaging, usually diagnostic mammography, is employed for women who do not wish to undergo elective surgery to remove DCIS tumors.
Nguyen and colleagues sought to evaluate what mammographic changes occur on DCIS surveillance, as well as the risk of invasive progression in women who do not undergo initial surgical excision following a new DCIS diagnosis.
In its study, the team included retrospective data collected between 2003 and 2022 from 52 women with an average age of 60.4 years. The women had a median follow-up of 3.6 years. They did not undergo surgery either because of personal preference or they were not eligible due to comorbidities. Out of the total, 36 women had low-risk DCIS cases while 16 had high-risk cases.
The researchers found that imaging changes on surveillance imaging prompted 33 biopsies in 19 women. Of these biopsies, 21 were false positives. Twelve women had DCIS progression to invasive ductal carcinoma; of these, invasive disease appeared as new calcifications in five women and new masses in five others, while the remaining two cases manifested as architectural distortion and nonmass enhancement. No patients with stable imaging were diagnosed with invasive ductal carcinoma, Nguyen's group noted.
Median time to invasive cancer progression was 3.6 years. The eight-year rate of such progression was 30%, Nguyen said. Progression to invasive disease occurred in seven out of 36 (19%) low-risk women and five of 16 (31%) high-risk women.
The researchers also found that women with low-risk DCIS who progressed to invasive ductal carcinoma had a more favorable biological profile. All seven women with low-risk DCIS who progressed had low or intermediate nuclear grade, luminal A (HR+, HER2-) invasive ductal carcinoma. Also, out of the five women with high-risk DCIS who progressed, three had luminal A and two had luminal B (HR+, HER2+) invasive ductal carcinoma.
Nguyen said that the study results suggest that close follow-up is critical in DCIS patients who undergo surveillance imaging. He added that risk category should be considered for women undergoing surveillance since low- and high-risk DCIS may differ in disease progression and outcomes.
"I think it really helps radiologists when they see new calcifications or new masses, that they can see they're suspicious and need a biopsy as early as possible to rule our invasive progression," he told AuntMinnie.com.