Most women are comfortable with having their mammogram data used to calculate lifetime breast cancer risk, suggest findings presented April 28 at the American Roentgen Ray Society annual meeting in San Diego, CA.
In her presentation, Liliana Light from Howard University in Washington, DC, discussed her team’s findings, showing that most women are also willing to pay more money for the use of newer breast cancer screening tools. Most respondents in the survey study also reported preferring to receive their risk reports from their gynecologists or primary care physicians rather than radiologists or genetic counselors.
“The results indicate that a significant percentage of women are concerned about their breast cancer risk and are interested in knowing their lifetime risk,” Light said.
The American College of Radiology and the Society of Breast Imaging recommend that women be assessed for lifetime breast cancer risk at 25 years old. The National Accreditation Program for Breast Centers requires risk assessment at the time of breast cancer screening or diagnosis. This puts supplemental screening via MRI or ultrasound more into focus.
With these updates and the development of new and more accessible screening tools in mind, Light and colleagues evaluated patient perspectives on breast cancer risk, assessment, and screening methods.
The team collected survey data from 319 women at medical departments specializing in radiology (n = 160), gynecology (n = 80), and internal medicine (n = 79).
On a scale of 1 (not concerned) to 5 (extremely concerned), 17.1% of respondents reported a score of 4 and 18% reported a score of 5 regarding concern for developing breast cancer. And 38.1% of the total respondents were interested in their lifetime risk of developing breast cancer, while 51.9% reported already knowing their risk.
Light also presented the following on behalf of the team:
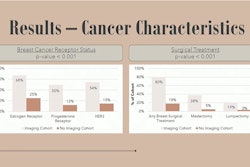
82.6% of respondents reported being comfortable with breast cancer risk being calculated from their screening mammograms; 31.7% felt comfortable having their personal or family history of breast cancer used.
Most of the women preferred getting their risk results from their gynecologist (n = 191), followed by their primary care physician (n = 161); 85 and 76 of the women preferred obtaining their results from their radiologist or genetic counselor, respectively.
Patients at the gynecology office preferred obtaining results from their gynecologist (p < 0.001), and at the internal medicine office, they preferred the radiologist (p = 0.006). The researchers reported no significant difference in preference at radiology offices.
49% of the women reported increased breast cancer risk. Of these respondents, 76.6% expressed interest in genetic testing, compared with 54.9% not at increased risk.
The researchers also found that 63.5% of the respondents reported being willing to pay out of pocket if insurance did not cover it. And 95.4% of the women showed interest in additional screening if they were found to be at higher risk. This included the following: breast MRI (68.8%), whole-breast ultrasound (61%), multicancer early detection blood tests (54.5%), and contrast-enhanced mammography (50.6%). For more screening tests, 55% of women at internal medicine offices were willing to pay more than $300 for these services compared with 50% of women at gynecology offices and 46.2% of women at radiology offices.
 In her presentation at ARRS 2025, Liliana Light discussed her team's findings showing that most women have positive attitudes toward mammography data being used to determine their breast cancer risk and toward newer screening options such as MRI and ultrasound.ARRS
In her presentation at ARRS 2025, Liliana Light discussed her team's findings showing that most women have positive attitudes toward mammography data being used to determine their breast cancer risk and toward newer screening options such as MRI and ultrasound.ARRS
While the cost of added testing may hinder some high-risk women seeking screening services, Light said the results further support expanding these services for women. She added that the finding of women willing to pay more for additional tests suggests that tests like whole-breast ultrasound and contrast imaging “may be of interest if appropriate and offered.”
“Most respondents preferred receiving their information on their risk from their primary care provider or their ob/gyn, highlighting the need for clear communication in healthcare settings,” she said.