FDG-PET imaging shows promise for use as a diagnostic criterion for neurosarcoidosis, with a recent case series illustrating the approach was effective when gold-standard approaches were not, according to a group of researchers in Berlin.
“To date, F-18 FDG PET findings are currently not taken into account when making a diagnosis for possible, probable, or definite neurosarcoidosis,” noted lead author Jessy Chen, MD, of Charité - Berlin University Medicine, and colleagues. The article was published January 25 in Neurological Research and Practice.
Neurosarcoidosis (NS) is a relatively rare form of sarcoidosis that affects the nervous system and is characterized by inflammation in the brain, spinal cord, and optic nerve. MRI is the imaging gold standard for diagnosis, yet identifying the disease using this method remains challenging, the researchers wrote.
F-18 FDG-PET is an established approach for diagnosing inflammation based on its ability to visualize increased cellular glucose metabolism, and the researchers hypothesized that it could be useful in patients with neurosarcoidosis.
To assess the concept, the researchers identified three patients between 2020 and 2022 at their hospital who had undergone MRI as well as additional F-18 FDG-PET scans to identify potential hypermetabolism in the central nervous system. In all three cases, gadolinium-enhanced MRI scans did not show abnormalities.
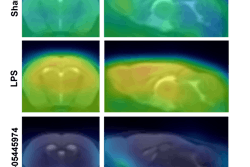
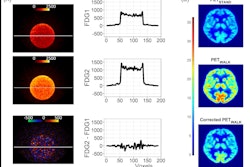
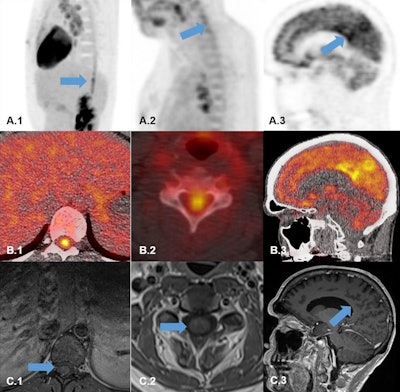 F-18 FDG-PET and MRI scans of three patients. (A.1-B.1) F-18 FDG-PET (A1 sagittal PET; B1 transaxial fused PET/CT) showing intense hypermetabolism in the lower thoracical spinal cord (blue arrow). (C.1) Transaxial MRI-scan (T1_TSE_FS) showing no abnormal gadolinium enhancement in the lumbar spinal cord (blue arrow). (A.2-B.2) F-18 FDG-PET (A2 sagittal PET; B2 transaxial fused PET/CT) showing hypermetabolism in the cervical spinal cord (blue arrow). (C.2) Transaxial MRI scan (T1_TSE_FS) showing no abnormal gadolinium enhancement in the cervical spinal cord (blue arrow). (A.3-B.3) F-18 FDG-PET (A3 sagittal PET; B3 transaxial fused PET/CT) showing bilateral hypermetabolism the precuneus region (blue arrow). (C.3) Transaxial MRI scan (T1_MPRAGE) showing no abnormal gadolinium enhancement in precuneus region (blue arrow). Image courtesy of Neurological Research and Practice.
F-18 FDG-PET and MRI scans of three patients. (A.1-B.1) F-18 FDG-PET (A1 sagittal PET; B1 transaxial fused PET/CT) showing intense hypermetabolism in the lower thoracical spinal cord (blue arrow). (C.1) Transaxial MRI-scan (T1_TSE_FS) showing no abnormal gadolinium enhancement in the lumbar spinal cord (blue arrow). (A.2-B.2) F-18 FDG-PET (A2 sagittal PET; B2 transaxial fused PET/CT) showing hypermetabolism in the cervical spinal cord (blue arrow). (C.2) Transaxial MRI scan (T1_TSE_FS) showing no abnormal gadolinium enhancement in the cervical spinal cord (blue arrow). (A.3-B.3) F-18 FDG-PET (A3 sagittal PET; B3 transaxial fused PET/CT) showing bilateral hypermetabolism the precuneus region (blue arrow). (C.3) Transaxial MRI scan (T1_MPRAGE) showing no abnormal gadolinium enhancement in precuneus region (blue arrow). Image courtesy of Neurological Research and Practice.
Conversely, the F-18 FDG-PET scans identified areas of increased F-18 FDG radiotracer uptake in the cervical and thoracic spinal cord in two patients and increased uptake within the brain’s precuneus area, bilaterally, in the third patient.
“We diagnosed all three patients with a ‘probable’ NS taking the positive F-18 FDG-PET scans as an imaging substitute for MRI results,” the group wrote.
In addition, the authors noted that in one previous study, 27 of 110 patients were diagnosed with possible, probable, or definite neurosarcoidosis based on F-18 FDG-PET imaging, with similar discordances between PET and MRI imaging.
Lastly, the authors noted that F-18 FDG-PET imaging led to successful outcomes for patients. Two of the patients were started on immunosuppressive treatment, which resulted in a remission of symptoms in one and visual improvement in the other, while the third patient underwent a treatment regime change.
“In our outpatient clinic follow-up (2 to 2.5 years depending on the patient case), all three patients remained stable without new disease relapses,” they noted.
Ultimately, the report describes three cases where F-18 FDG-PET was relevant for the diagnosis of neurosarcoidosis, underscoring the question of whether the technique “should be considered as a criterion for NS,” the group concluded.
The full study is available here.