F-18 FDG-PET imaging in patients with dementia with Lewy bodies (DLB) has shown that brain hypo- and hypermetabolism may have different effects on cognition, according to a study published January 3 in npj Parkinson’s Disease.
The study is the first to show that these brain glucose metabolism patterns may independently affect cognitive decline and to clarify potential therapeutic targets in these patients, according to the authors.
“The present study suggests that DLB-hypo and DLB-hyper may be independent of each other and differentially affect the baseline and longitudinal cognitive function in patients with DLB,” wrote lead authors Seong Ho Jeong, a PhD candidate at Yonsei University College of Medicine in Seoul, South Korea, and Jungho Cha, PhD, of the Icahn School of Medicine at Mount Sinai in New York City.
DLB is the second most common neurodegenerative dementia after Alzheimer’s disease. Previous F-18 FDG-PET studies have shown that hypometabolism and hypermetabolism are present in different areas of the brain in these patients, the authors explained.
However, although the brain areas showing relative hypometabolism and hypermetabolism have been detected concurrently in individuals with DLB, no study has investigated whether the hypo- and hypermetabolic areas are coupled or independent of each other, they noted.
Thus, in this study, the group investigated the relationship between these patterns and cognitive function in patients.
The researchers enrolled 55 patients with DLB (15 with prodromal DLB and 40 with probable DLB) and 13 healthy controls who underwent F-18 FDG-PET and detailed neuropsychological tests. They used a linear mixed model to identify associations between different brain areas affected by hypometabolism and hypermetabolism and changes in longitudinal cognitive decline.
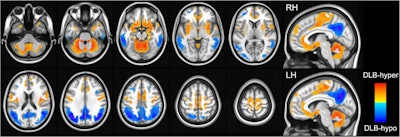 DLB-hypo (hypometabolic changes in dementia with Lewy bodies) was characterized by relatively reduced bilateral metabolic activity (color-coded blue) in the bilateral parietal, temporal, and occipital cortices, while DLB-hyper (hypermetabolic changes in dementia with Lewy bodies) showed relatively increased metabolic activity (color-coded red) in the cerebellum, bilateral sensorimotor, orbitofrontal, insular, and parahippocampal cortices, bilateral putamen, globus pallidum, hippocampus, and amygdala. Image courtesy of npj Parkinson’s Disease.
DLB-hypo (hypometabolic changes in dementia with Lewy bodies) was characterized by relatively reduced bilateral metabolic activity (color-coded blue) in the bilateral parietal, temporal, and occipital cortices, while DLB-hyper (hypermetabolic changes in dementia with Lewy bodies) showed relatively increased metabolic activity (color-coded red) in the cerebellum, bilateral sensorimotor, orbitofrontal, insular, and parahippocampal cortices, bilateral putamen, globus pallidum, hippocampus, and amygdala. Image courtesy of npj Parkinson’s Disease.
According to the findings, DLB-hypo was associated with language, visuospatial, visual memory, and frontal/executive functions, while DLB-hyper was responsible for attention and verbal memory. In addition, a linear mixed model showed that DLB-hypo was associated with longitudinal cognitive outcomes, regardless of cognitive status, and DLB-hyper contributed to cognitive decline only in patients with mild cognitive decline, they wrote.
“DLB-hypo and DLB-hyper may differentially and independently affect baseline and longitudinal cognitive functions in patients with DLB,” the researchers wrote.
Ultimately, most previous studies have examined patterns of cerebral glucose metabolism without considering independent roles for hypermetabolism and hypometabolism in cognitive function in Lewy body spectrum disorders, the authors noted. As the first study to suggest differences in these patterns and cognitive function in patients, the study was limited, namely by the small sample size, and further research is warranted, they added
“Our findings imply that further studies investigating whether brain hypermetabolism in DLB can be a therapeutic target are warranted,” the group concluded.
The full article can be found here.




















