Photon-counting CT (PCCT) has a better safety profile for lung cancer imaging compared with energy-integrating detector CT (EID-CT), according to research published February 3 in Radiology.
PCCT led to lower radiation exposure, fewer adverse reactions, and lower rates of contrast-induced acute kidney injury compared with EID-CT, reported a team led by Yuhan Zhou, MD, from the First Affiliated Hospital of Zhengzhou University in China.
“The PCCT images, especially with a 0.4-mm section thickness, improved overall image quality, detection of enhancement-related malignant features, and diagnostic confidence, making it suitable for various body mass index and small lesions,” the Zhou team wrote.
While contrast-enhanced chest CT is recommended for tumor characterization in lung cancer patients, prior reports express concern about cumulative radiation exposure and adverse side effects of contrast agents on some patients.
Some strategies to reduce radiation exposure with EID-CT include decreasing tube current and/or voltage, increasing pitch, and improving detector sensitivity. PCCT, meanwhile, directly converts x-ray photons into electrical signals through electron-hole pair generation, improving spatial resolution while improving geometric dose efficiency.
The researchers noted a lack of data on finding contrast enhancement-related malignant features and applicable scenarios for low-dose ultrahigh-resolution PCCT in lung cancer imaging. Zhou and colleagues compared the benefits of PCCT versus EID-CT at contrast-enhanced chest CT for different lung cancer patient populations.
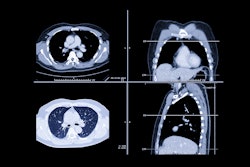
 Subgroup analysis based on lesion size on PCCT images. The red outlined areas highlight the magnified images of lesions. (A-C) PCCT images in a 62-year-old woman with a body mass index (BMI) of 23.6, calculated as weight in kilograms divided by height in meters squared, who was diagnosed with adenocarcinoma. A lesion with a long diameter of 25 mm was identified in the right lower lobe on axial images acquired during the venous phase. For lesions less than or equal to 30 mm, decreasing section thickness improved boundary sharpness and contrast between the necrotic area and enhanced tissue, with optimal visualization at 0.4 mm. (D-F) PCCT images in a 66-year-old man with a BMI of 24.2 who was diagnosed with adenocarcinoma, revealing a lesion with a long diameter of 52 mm in the right lower lobe. For lesions greater than 30 mm, a section thickness of 1 mm demonstrated better contrast and clarity at the boundary of the necrotic area compared with 0.4 mm. This observation supported the selection of an appropriate section thickness for accurate quantification of necrotic regions within the lesion.RSNA
Subgroup analysis based on lesion size on PCCT images. The red outlined areas highlight the magnified images of lesions. (A-C) PCCT images in a 62-year-old woman with a body mass index (BMI) of 23.6, calculated as weight in kilograms divided by height in meters squared, who was diagnosed with adenocarcinoma. A lesion with a long diameter of 25 mm was identified in the right lower lobe on axial images acquired during the venous phase. For lesions less than or equal to 30 mm, decreasing section thickness improved boundary sharpness and contrast between the necrotic area and enhanced tissue, with optimal visualization at 0.4 mm. (D-F) PCCT images in a 66-year-old man with a BMI of 24.2 who was diagnosed with adenocarcinoma, revealing a lesion with a long diameter of 52 mm in the right lower lobe. For lesions greater than 30 mm, a section thickness of 1 mm demonstrated better contrast and clarity at the boundary of the necrotic area compared with 0.4 mm. This observation supported the selection of an appropriate section thickness for accurate quantification of necrotic regions within the lesion.RSNA
The study included 200 participants (average age, 61.6) with lesions who in 2024 underwent either low-dose contrast PCCT (1 mL/kg at 2 mL/sec) or standard-dose EID-CT (1.2 mL/kg at 3 mL/sec). The team constructed images into five-section thicknesses: 5 mm, 1 mm, and 0.4 mm for PCCT and 5 mm and 1 mm for EID-CT.
PCCT led to a 66.3% reduction in radiation and a 26.6% reduction in iodine exposure. It also lowered adverse reactions and contrast-induced acute kidney injury.
Comparison between PCCT, EID-CT | |||
Measure | EID-CT | PCCT | p-value |
Radiation exposure | 4.04 mSv | 1.36 mSv | < 0.001 |
Iodine exposure | 28.08 mg | 20.62 mg | < 0.001 |
Adverse reactions | 9% | 2% | < 0.001 |
Contrast-induced acute kidney injury | 7% | 1% | < 0.001 |
The team also used a 5-point Likert scale to analyze lesion image quality, with a score of 5 being the highest quality.
It found that PCCT imaging at 0.4 mm showed higher detection and diagnostic confidence for enhancement-related malignant features (Likert 5 vs. Likert 3; p < 0.001) and yielded higher overall image quality (Likert 5; p < 0.05) in normal-weight participants. PCCT also had higher image quality for structures within enhanced lesions of less than or equal to 3 cm (Likert 4 vs. Likert 3; p < 0.001).
The study authors called for future research to include longitudinal follow-up scans within the same participants. This would help evaluate the advantages of contrast-enhanced EID-CT and PCCT in long-term lung cancer monitoring and treatment assessment.
“Another potential area for future evaluation is the utilization of virtual monoenergetic images to address the issue of decreased vascular CT attenuation caused by low contrast agent dose,” they wrote.
Read the full study here.