Thoracic radiologists from multiple international institutions and societies have collaborated on new guidelines for best practices in CT imaging for patients with post-COVID lung abnormalities.
A team led by Soon Ho Yoon, MD, PhD, of Seoul National University Hospital in South Korea, sought to standardize recommendations for the appropriate use of chest CT in patients with residual lung abnormalities following COVID infection. The consensus statement was published July 22 in Radiology.
The authors recommend chest CT for patients whose respiratory symptoms continue or worsen three months after infection and have lasted for at least two months with no other explanation. Given the high rate of residual lung abnormalities in patients who have been hospitalized with moderate or severe COVID-19, chest CT administered three to six months after discharge for these patients should also be considered.
According to the guidance, the interval and frequency of CT follow-ups should be guided by both clinical judgment and radiological expertise, and based on the extent of initial lung abnormalities, temporal changes, and pulmonary physiology.
Moreover, the guidance recommends adherence to the “as low as reasonably achievable” (ALARA) principle for low-dose protocols in serial CT follow-up. However, the authors stated that ultralow-dose CT (<0.5 mSv) is not advised for evaluating residual post-COVID-19 residual lung abnormalities, stressing that ground-glass opacities, which are common, often cannot be assessed accurately with ultralow-dose scans.
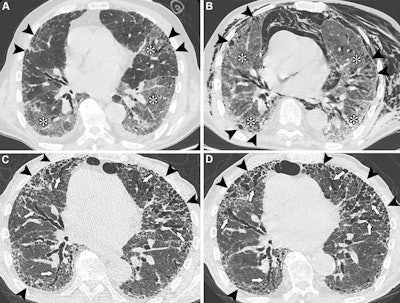 Unenhanced axial CT images show COVID-19 pneumonia in an 83-year-old male patient with preexisting interstitial lung disease (ILD). (A) Image shows ground-glass opacities in the lower lobes and in the lingula (*). Irregular reticular opacities with mild distal traction bronchiectasis are evident in the subpleural regions of both upper lobes (arrowheads), suggesting preexisting ILD with a probable usual interstitial pneumonia pattern. (B) Image obtained during hospitalization for respiratory distress shows spontaneous pneumomediastinum and diffuse chest wall subcutaneous emphysema, predominantly on the left side. The image also shows persistent, diffuse ground-glass opacities (*) and peripheral fibrotic lung changes (arrowheads). (C) Unenhanced follow-up image obtained at six months shows the progressive nature of lung fibrosis, with the development of honeycombing (arrowheads) and severe bronchiectasis (arrows), predominantly affecting the anterior peripheral regions of both lungs. (D) Unenhanced follow-up image obtained at 14 months shows the progression of honeycombing (arrowheads) and severe bronchiectasis (arrows) at the anterior peripheral regions of both lungs. In this case, SARS-CoV-2 infection likely acted as a trigger for the exacerbation of previously undiagnosed fibrotic ILD, with mechanical ventilation potentially contributing to extensive fibrosis in the anterior lung regions (arrowheads). The patient was administered antifibrotic therapy after the resolution of the acute phase.RSNA
Unenhanced axial CT images show COVID-19 pneumonia in an 83-year-old male patient with preexisting interstitial lung disease (ILD). (A) Image shows ground-glass opacities in the lower lobes and in the lingula (*). Irregular reticular opacities with mild distal traction bronchiectasis are evident in the subpleural regions of both upper lobes (arrowheads), suggesting preexisting ILD with a probable usual interstitial pneumonia pattern. (B) Image obtained during hospitalization for respiratory distress shows spontaneous pneumomediastinum and diffuse chest wall subcutaneous emphysema, predominantly on the left side. The image also shows persistent, diffuse ground-glass opacities (*) and peripheral fibrotic lung changes (arrowheads). (C) Unenhanced follow-up image obtained at six months shows the progressive nature of lung fibrosis, with the development of honeycombing (arrowheads) and severe bronchiectasis (arrows), predominantly affecting the anterior peripheral regions of both lungs. (D) Unenhanced follow-up image obtained at 14 months shows the progression of honeycombing (arrowheads) and severe bronchiectasis (arrows) at the anterior peripheral regions of both lungs. In this case, SARS-CoV-2 infection likely acted as a trigger for the exacerbation of previously undiagnosed fibrotic ILD, with mechanical ventilation potentially contributing to extensive fibrosis in the anterior lung regions (arrowheads). The patient was administered antifibrotic therapy after the resolution of the acute phase.RSNA
“Follow-up imaging plays a key role in assessing these residual changes and guiding clinical care, but it should be performed judiciously," said senior author Anna Rita Larici, MD, of Agostino Gemelli University Polyclinic Foundation in Rome, in a statement released by the RSNA. "Adherence to established recommendations helps ensure that patients receive follow-up imaging and care only when clinically indicated."
In addition to suggestions for CT acquisition in these patients, the authors also recommend using standardized, precise terminology in reporting to describe the diverse manifestations of lung damage after COVID-19 infection. If there is suspicion of a preexisting interstitial lung disease (ILD), this would include making the distinction between CT lung abnormalities presumed to be related to COVID-19 infection and those related to the ILD, according to the guidelines.
Not only does making these distinctions avoid confusion, it also enables healthcare providers to make better-informed decisions about patient management, as well as providing accurate data for future research, Larici added.
The guidance will prove to be a useful resource, according to an accompanying commentary.
"This best-practice consensus statement regarding post–COVID-19 abnormalities at CT will be a valuable reference for radiologists, allowing for consistent clinical reporting and standardization of reporting in future research," noted Loren Ketai, MD, professor emeritus of thoracic radiology at the University of New Mexico Health Science Center in Albuquerque.
Read the full guidance here.