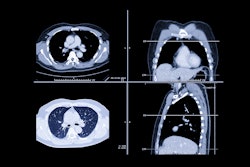
Changing national lung cancer screening guidelines in 2021 may have contributed to a surge in screening exams, but less lung cancer was detected in newly screened participants, and racial, ethnic, and sexual disparities persisted overall, according to a study published July 21 in the Journal of Thoracic Imaging.
While numerous studies have examined the effects of the U.S. Preventive Services Task Force (USPSTF)'s 2021 lung cancer screening (LCS) guidelines on eligibility, this study focused on participation and lung cancer outcomes over the first 10 years of implementing an LCS program.
Led by Yannan Lin, MD, PhD, of the David Geffen School of Medicine at the University of California, Los Angeles (UCLA), a team of researchers hypothesized that patients undergoing LCS after the release of the USPSTF's updated guidelines would be younger, more racially and ethnically diverse, and have a reduced smoking history.
"Adoption of [low-dose CT] LDCT screens has increased over time," noted the study authors, who estimated that from 2015 to 2020, the LCS program at UCLA served from 20 to 40 new patients monthly, then tripled in participation following the release of new guidelines in March 2021 (68 vs. 23, p < 0.05).
Lin and colleagues' study analyzed screening eligibility, participation, and lung cancer-related outcomes for 3,929 individuals who underwent LDCT screening between July 2013 and August 2023. Considering data relative to the USPSTF's previous LCS guideline in 2013, researchers extracted electronic health record (EHR) information and defined newly eligible patients as those who met the 2021 but not the 2013 USPSTF guidelines.
Participants fell into preguideline (1,963) and postguideline (1,966) groups based on baseline LDCT screen date, insurance status, and LCS eligibility.
Lin and colleagues did find that participants were slightly younger in the postguideline group, and they had a reduced smoking history. However, the proportions of race and ethnicity categories were statistically different between the preguideline and postguideline revision groups (p < 0.05). The postguideline revision group consisted of a slightly higher proportion of Hispanic patients (7.6% vs. 5.5%), fewer Black (5.1% vs. 6.9%), and fewer white patients (71.6% vs. 77%), the team reported.
"Simply revising the guidelines increases eligibility but does not guarantee participation in LCS for these populations," Lin and colleagues wrote. "These findings underscore the need for continued emphasis on active outreach and patient education efforts to promote LCS among racial and ethnic minority groups, as well as the further evaluation of how these initiatives impact participation and outcomes."
The team also observed a notable increase in the proportion of negative (i.e., Lung-RADS 1 or 2) LDCT screening results in the postguideline revision group compared with the preguideline revision group (89.4% vs. 84.5%, p < 0.05). Approximately half (48%) of the postguideline revision group patients were newly eligible (943), they noted.
Participants in the postguideline revision group had a lower mean PLCOm2012 risk score for lung cancer, compared to the preguideline revision group, the group explained. There were 89 and 17 patients with lung cancers in the preguideline and postguideline revision groups, respectively.
Read the complete study here.