Hamartoma:
View cases of pulmonary hamartoma
Clinical:
A hamartoma is the most common benign lung tumor, although it is a relatively uncommon lesion (incidence of pulmonary hamartomas in the general population is 0.25% [4]). It is likely an acquired lesion, derived from the peribronchial mesenchyme [4]. Patients are typically 50-60 years old and males are affected more than female (3:1). Patients are generally asymptomatic (90%) and the lesion is almost always solitary. The lesion is usually peripheral (subpleural), but 10% are central and 1.4 to 3% are endobronchial [5,6] (although other authors suggest that up to 10-20% are endobronchial [7]). It has been reported that hamartomas grow slowly at a rate of 1.5 mm per year and double in size about every 14 years [2]. Histologically, hamartomas are composed of both mesenchymal (cartilage) and epithelial elements.
Carney's Syndrome is characterized by multiple chondromatous
pulmonary hamartomas, leiomyoma (sarcoma) of the stomach, and
extra-adrenal paragangliomas. It is typically seen in female
patients under the age of 20 years [4].
Cowden disease/syndrome
(multiple hamartoma syndrome) is also associated with multiple
hamartomas. Cowden syndrome is an autosomal dominant disorder
caused by germline mutations in the phosphate and tensin homolog
(PTEN) gene (chromosome 10q23) [8]. PTEN is a tumor suppressor
gene which plays an important role in cell regulation and
apoptosis by negatively regulating the phosphoinositide 3-kinase
signaling pathway [8]. Breast cancer is the most common malignancy
seen in Cowden syndrome with a life time risk of 77% at age 70
years [8]. Non-medullary thyroid cancer is the second most common
malignancy with a lifetime risk of 38%, most commonly papillary
thyroid cancer [8]. These patients are also at increased risk for
papillary renal cell carcinoma (28%), endometrial cancer (34%),
and colorectal cancer (up to 20%) [8].
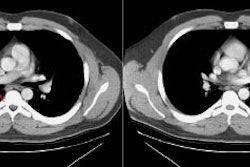
X-ray:
On CXR the lesion is usually sharply marginated and calcification is identified in 10-25% of lesions with a classic popcorn, curvilinear, or stippled appearance. Fat is seen in 30-50% of lesions on CT and is diagnostic of a hamartoma. On MRI, hamartomas have intermediate signal on T1 and high signal on T2 and can have a lobulated appearance. Contrast enhancement of internal septa (branching mesenchymal connective tissue that dips into the cartilagenous core) has been identified [1].
REFERENCES:
(1) J Thorac Imag 1995; The bronchi: an imaging perspective. 10: 236-254 (p.243)
(2) Radiographics 1998; Meyer CA, White CS. Cartilagenous disorders of the chest. 18: 1109-1123
(3) AJR 1999; Thomas JW, et al. Pulmonary hamartoma. 172: 1643 (No abstract available)
(4) Cancer 1999; Kiryu T, et al. Multiple chondromatous hamartomas of the lung. A case report and review of the literature with special reference to Carney syndrome. 85: 2557-61
(5) AJR 2006; Ko JM, et al. Benign tumors of the tracheobronchial tree: CT-pathologic correlation. 186: 1304-113
(6) Radiographics 2008; Martinez S, et al. Mucoid impactions:
finger-in-glove sign and other CT and radiographics features. 28:
1369-1382
(7) AJR 2013; Ngo VH, et al. Tumors and tumorlike conditions of
the large airways. 201: 301-313
(8) Radiographics 2019; Tiwari R, et al. Radiologist's primer on
imaging of common hereditary syndromes. 39: 759-778