Pulmonary Lymphangitic Carcinomatosis:
Clinical:
In most cases the tumor disseminates hematogenously to the lungs and only secondarily penetrates the vessel walls and invades the surrounding interstitium and lymphatics [2]. Thus, the tumor spreads from the lung periphery centrally via the interstitium around the lymphatics. In about 25% of patients, pulmonay lymphangitic carcinomatosis occurs as a result of retrograde spread from the tumor-laden hilar lymph nodes [2].The most common malignancy associated with lymphangitic mets is bronchogenic carcinoma- most commonly adenocarcinoma (particularly if unilateral), followed by breast, GI malignancies (stomach and colon), and prostate cancer [2,3]. About 80% of tumors associated with lymphangitis mets are adenocarcinomas. Patients commonly experience progressive dyspnea/shortness of breath [2], occasionally dry cough and hemoptysis [2], have widened alveolar-arterial oxygen gradients, and restrictive defects on pulmonary function testing. Lymphangitic mets are associated with a very poor prognosis, frequently with death within 6 months.
X-ray:
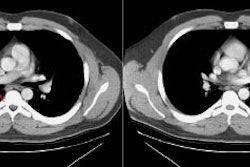
CXR may be normal (in up to 50% of cases), or demonstrate a reticular or mixed reticulonodular pattern or thickening of the perihilar bronchial vasculature [2]. A pleural effusion is found in 60% of cases. Hilar adenopathy is noted in less than 25-50% of cases.Chest CT is more specific and sensitive than CXR for the diagnosis of lymphatic mets [2]. On HRCT there is variable, smooth, irregular, or nodular thickening of the interlobular septae and bronchovascular bundles which often have a beaded appearance. The septal thickening outlines the pulmonary lobules producing "polygonal arcades [2]." Another characteristic feature is either smooth or nodular thickening of the peribronchovascular interstitium. Similar changes can be seen along the fissures. In many patients the abnormality is unilateral (30-50%) or patchy, sparing some areas of lung. Pleural effusion is found in 30-50% of patients [2]. Hilar adenopathy is found in 30-50% of cases [2].
Patients with lymphangitic carcinomatosis due to extrathoracic malignancies have bilateral abnormalities at presentation in up to 80-90% of cases.
An important finding is that the normal lung architecture is preserved, honeycombing is NOT a feature associated with this condition.
Differential considerations: Smooth septal thickening can be seen with pulmonary edema. Nodular septal thickening is also seen with sarcoid, silicosis, and coal workers pneumoconiosis- however, these disorders are associated with architectural distortion.
REFERENCES:
(1) AJR 1992; Johkoh T, et al. CT findings in lymphangitic carcinomatosis of the lung: Correlation with histologic findings and pulmonary function tests. 158: 1217-1222
(2) AJR 2010; Prakash P, et al. FDG PET/CT in assessment of pulmonary lymphangitic carcinomatosis. 194: 231-236
(3) Radiographics 2011; Nair A, et al. Revisions to the TNM staging of non-small cell lung cancer: rationale, clinicoradiologic implications, and persistent limitations. 31: 215-238