Hodgkins Lymphoma:
Clinical:
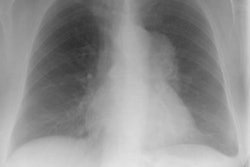
Hodgkins lymphoma (HL) is the most common mediastinal lymphoma, however, it accounts for only about 20-30% of all lymphomas. Four histologic subtypes are described in the Rye classification system: nodular sclerosing (75-80%, the most common cell type), lymphocyte predominant (10%), mixed cellularity (10%), and lymphocyte depleted (5%). Pathologically, the diagnosis of HL is established by the identification of Reed-Sternberg cells. Patients with HL tend to present with cervical or supraclavicular adenopathy, and about 20-30% will have fever, night sweats, and/or weight loss (referred to as "B" symptoms). There is a bimodal incidence between 20-30 years, and again at 50 years. Patients with mediastinal disease tend to be younger than those without mediastinal disease (4). Although up to 85% of patients with Hodgkins have intrathoracic disease, isolated mediastinal disease is uncommon (10%) and there is typically adenopathy elsewhere. Only 15% of patients with intrathoracic HL have enlargement of a single lymph node group and only rarely are the posterior or paracardiac lymph node groups involved. Contiguous spread from one group of lymph nodes to the next occurs predictably.
Treatment is radiation therapy (XRT) alone for Stage I or II non-bulky disease. Patients with Stage III or IV disease typically receive chemotherapy which may be combined with XRT. Overall, the cure rate is greater than 90% for Stage I or II disease, between 60-80% for stage III, and 50-60% for stage IV. Prognosis is in part dependent upon cell type with the lymphocyte predominant histologic subtype having the best prognosis (LP>NS>MC>LD). In general, any mediastinal mass in a Hodgkin's patient worsens the prognosis, especially if it is greater than one third of the thoracic diameter. Direct invasion of the adjacent lung also worsens the prognosis.
Pulmonary parenchymal involvement can be found in up to 12% of patients [4] and is almost invariably associated with hilar/mediastinal nodal disease (fewer than 100 cases isolated to the lung at presentation have been reported). The most common finding described in primary pulmonary Hodgkins disease is a single or multiple nodules. Hodgkins disease can also present as an endobronchial mass.
Patients may relapse with pulmonary disease without associated adenopathy. Patients are frequently asymptomatic. In fact, pulmonary involvement will eventually occur in 30-40% of patients with Hodgkins disease. The most common finding is multiple nodules which may contain air-bronchograms. Other findings include lobar or segmental consolidations with air bronchograms that may be indistinguishable from pneumonia (much less common), or a reticular pattern with septal lines due to lymphatic/venous obstruction by bulky adenopathy or from intrinsic tumoral deposits within interstitial lymphatic pathways. Pleural effusions are commonly present.
Staging:
Stage I: Involvement of one nodal site Stage II: Involvement of more than one nodal site, limited to one side of the diaphragm Stage III: More than one nodal site, both sides of the diaphragm Stage IV: Metastatic disease "S" designation indicates splenic involvement "E" designation indicates local extension
X-ray:
Computed Tomography: CT can detect intrathoracic sites of disease not detected on CXR in up to 20% of patients. The effect on patient management is quite variable (between 10-60% of patients), and is related to the specific protocol for which the patient is being considered. On CT there is usually an asymmetric, anterior mediastinal soft tissue mass which may invade the chest wall. Bulky mediastinal nodal disease can be associated with interstitial edema due to lymphatic/venous obstruction. Although typically homogeneous, larger masses may contain areas of decreased attenuation representing necrosis or cyst formation. Calcification is RARE prior to therapy. A pleural effusion is seen in up to 30% of cases and is usually felt to be related to lymphatic/venous obstruction from the mediastinal mass [ACR Syllabi #40:p.134 suggests effusions are found in only 2% of cases]. Benign pericardial effusions may also be seen in such patients.
|
|
|
|
*Significant decrease in size of nodal disease has been reported in association with steroid premedication prior to CT scanning. This may be related to activity steroids have been shown to have in the treatment of Hodgkin's lymphoma (steroids are used in some treatment regimens for lymphoma). The use of steroid premedication should be avoided in patients with suspected lymphoma or during patient follow-up [5].
Magnetic Resonance Imaging: In adults, the normal thymus has a homogeneous signal intensity close to that of fat. On MRI, lymphoma typically demonstrates a homogeneous low signal intensity similar to muscle on T1 images, and high (greater than fat) or mixed signal on T2. During treatment, the signal intensity will change [7]. Active, untreated tumor cointains an excess of free water, which increases the signal intensity on T2 images [7]. With successful treatment, cellular elements and the water content of the tumor are reduced, while collagen and fibrotic stroma increase [7]. These factors reduce the signal intensity of any residual mass on T2 images [7]. Variable gadolinium enhancement can be seen prior to treatment and the degree of enhancement typically decreases following successful therapy [7].
Scintigraphy:
Hodgkin's: Gallium-67 scanning- about 90% of Hodgkin's lymphomas are gallium avid pre-treatment. Lymphocyte predominant tumors (which account for only 10% of cases) are less gallium avid (79%). SPECT imaging has a sensitivity of 95% and a specificity of 90% for the detection of mediastinal disease in Hodgkin's lymphoma. The gallium exam is not useful for assessing splenic involvement. The periportal area may also be difficult to assess.
Positron Emission Tomography: See PET imaging section
REFERENCES:
(1) AJR 1997; Au V, Leung AN. Radiologic manifestations of lymphoma in the thorax. 168: 93-98 (No abstract available)
(2) AJR 1997; Imaging of pulmonary lymphomas.168: 339-345 (No abstract available)
(3) Radiology 1997; 203: 795-800
(4) Chest 1997; Strollo DC, et al. Primary mediastinal tumors. Part II. Tumors of the middle and posterior mediastinum. 112: 1344-57
(5) AJR 1998; Wong TZ. Streroid premedication before IV contrast-enhanced CT resulting in resolution of adenopathy. 170: 218 (No abstract available)
(6) J Nucl Med 1997; 38 (3): 343-348
(7) Radiology 2001; Rahmouni A, et al. Mediastinal lymphoma: Quantitative changes in gadolinium enhancement at MR imaging after treatment. 219: 621-628