Beryliosis:
Clinical:
Beryliosis is a chronic, granulomatous systemic disease
(involves liver, skin, etc...) with primary pulmonary involvement
that mimics sarcoidosis. The disoder represents a granulomaotous
hypersensitivity response to inhaled beryllium [3]. Berylliosis is
uncommon and only seen in individuals who have industrial exposure
(ceramics industry, fluorescent lamp manufacturing, aerospace and
nuclear weapons production [4]). Chronic beryllium disease
develops in up to 16% of exposed workers [2]. The berylium
particle is typically inhaled, but a secondary portal of entry is
the skin. Patients present with dyspnea, cough, fever, anorexia,
weight loss, contact dermatitis, and non-healing ulcers. The
incidence of the disorder and the severity are not always related
to the intensity and duration of exposure - in fact, it may occur
with relatively minimal exposure (particularly in those with a
genetic predisposition) [3].
On histologic analysis, non-caseating granulomas identical to those found in sarcoid are identified. The berylium particles themselves must be located in order to distinguish the disorder from sarcoid. Treatment of symptomatic patients consists of prolonged corticosteroid therapy [2].
Spontaneous pneumothorax occurs in slightly more than 10% of affected patients. An acute form of beryliosis may occur due to acute high exposure which produces a chemical pneumonitis with an acute alveolar pattern on CXR. In this form of the disorder, alveolar wall damage results in an acute pulmonary edema type pattern.
X-ray:
CXR is often normal in early-stage disease [2]. Abnormalities are seen in about 50% of cases and are generally characterized by small nodules or reticulonodular opacities that predominate in the mid and upper lung zones [2]. Moderate nodal enlargement is frequent [2], but other authors suggest that mediastinal and hilar adenopathy are less common- occurring in about 25% of cases- and less severe [3,4]. The findings produce a pattern indistinguishable from sarcoid. In more advanced disease, coalescence of granulomatous lesions can produce larger masses and interstitial fibrosis and honeycombing are also seen [2].
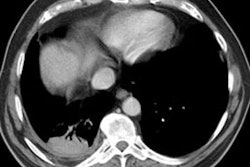
On CT, the most common finding is small parenchymal nodules (about 57% of cases) distributed along bronchovascular bundles or interlobular septa [2]. Interlobular septal thickening is seen in about 50% of cases [2]. Other findings include ground glass opacities (32%), honeycombing, and conglomerate mass [2]. Hilar or mediastinal adenopathy is observed in about 40% of cases [2].
REFERENCES:
(1) Radiol Clin North Am 1991; Sep. 29(5): p.931-41
(2) Radiographics 2006; Chong S, et al. Pneumoconiosis:
comparison of imaging and pathologic findings. 26: 59-77
(3) Radiology 2014; State of the art: imaging of occupational
lung disease. 270: 681-69
(4) AJR 2020; Lee GM, et al. Sarcoidosis: a diagnosis of exclusion. 214: 50-58