Pancreatic-Renal Transplant:
Clinical:
Kidney-pancreas transplants are done with increasing frequency in patients with poorly controlled diabetes in an effort to restore normal endocrine function of the pancreas and prolong renal transplant survival (5 year graft survival is 80%). A short segment of duodenum associated with the pancreatic transplant is anastamosed to the dome of the bladder so that exocrine secretions can be eliminated.
Pancreatic graft complications:
In combined pancreas and renal transplants, pancreatic graft survival is inferior to renal graft survival. This is most likely related to a higher incidence of complications such as thrombosis and pancreatitis.
Acute Pancreatic Rejection:
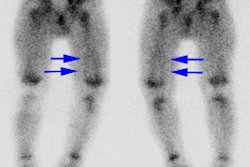
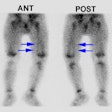
Up to 60% of pancreatic transplants develop graft rejection. Pancreatic rejection occurs synchonously with renal transplant rejection in about 50% of cases, while isolated pancreatic rejection is identified in 15-25% of cases. Clinical detection of pancreatic transplant failure is difficult because physical and laboratory signs (such as hypoamylasuria) cannot accurately diagnose early pancreatic dysfunction. Tc-HMPAO extraction is proportional to blood flow, and may have a role in evaluation of graft function. Lack of Tc-HMPAO accumulation in the transplant indicates either vascular thrombosis or graft pancreatitis.
On ultrasonography, the most common finding in acute rejection is pancreatic enlargement (sensitivity 58%, specificity 100%). Other findings include loss of marginal definition, focal or diffuse areas of decreased echogenicity, and the presence of peripancreatic fluid collections, however, these findings are very non-specific as they can also be seen in cases of pancreatitis and ischemia. An increase in the resistive index (greater than 0.7) has also been reported (sensitivity 20%, specificity 73%). Unfortunately, gray scale and doppler sonography are inferior to sonographically guided percutaneous biopsy. Complication rates from the procedure are low (under 2%) and a diagnosis can be obtained in 88-95% of cases. [1].
MRI can also be used to assess for pancreatic rejection [2].
Vascular Complications:
Graft thrombosis, including both venous and arterial, is second only to rejection as a cause of graft failure after pancreatic transplantation (5-14% of transplants). Venous thrombosis can lead to hemorrhagic pancreatitis, organ necrosis, infection, and thrombus propagation.
1. Venous thrombosis: Venous thrombosis is estimated to occur in 5% of pancreatic transplants. Predisposing factors include underlying coagulopathy, long preservation time of the transplant, poor quality native donor vessels, left sided graft placement, and use of a venous extension graft. Venous thrombosis can be difficult to diagnose. Clinical signs and symptoms are non-specific. Abnormally high-resistance arterial flow and flow reversal in diastole can be seen. Reversal of diastolic flow in pancreatic transplant arteries is highly specific for detection of graft venous thrombosis during the first 12 days after transplantation. A resistive index greater than or equal to 1.00 and absence of venous flow help to confirm the diagnosis. [3]
Urine Leak following Pancreatic Transplant:
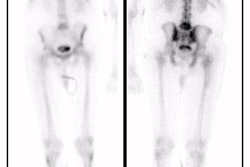
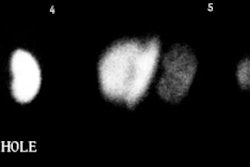
Urine leak from the duodenal segment which occurs in 9 to 14% of cases. Such leaks may occur at any time after the procedure- even as late as 5 years after tranplantation. Technetium VCUG has been shown to be more sensitive than conventional VCUG in the detection of such leaks due to superior detection of leaks on the post-void images [4].
REFERENCES:
(1) AJR 1996; 166:803-807
(2) Radiology 1999; Krebs TL, et al. Acute pancreatic transplant rejection: evaluation with dynamic contrast-enhanced MR imaging compared with histopathologic analysis. 210: 437-442
(3) AJR 1997; Diagnosis of venous thrombosis by duplex sonography. 169: 1269-1273
(4) AJR 1995; Aug. p.349-354