MONTEREY, CA - Ultrasound can be a useful tool for evaluating the nodal basins in breast cancer patients, while reducing unnecessary axillary node dissections. For the past decade, sonography has been successfully incorporated into the protocol for breast cancer staging at the M.D. Anderson Cancer Center in Houston.
Dr. Bruno Fornage described the benefits of sonographic lymph node exploration on Tuesday at the 2001 Breast Imaging Conference, which is sponsored by Instrumentarium Imaging. Fornage is a professor of diagnostic radiology and surgical oncology at M.D. Anderson.
"Staging of breast cancer includes the tumor size, and the tumor size is the most important prognostic factor, along with nodal involvement," Fornage said. "Another thing that we want to tell the surgeon, or whoever is going to be treating patients, is if the lesion is unifocal or multifocal. We need to assess the lymphatic spread of the tumor. Mammography has not been good at that. Ultrasound has some value in this application."
Specifically, ultrasound is employed to assess the ipsilateral axilla and internal mammary chain of vessels along the sternum.
"When we find a [metastatic] internal mammary lymph node on the same site of the cancer, this is going to be rated as an N3. N3 means that your patient is at Stage IIIB, regardless of the site of the primary tumor. That’s how ultrasound can refine the [cancer] staging of your patients," Fornage said. "So what is the metastasis going to look like? We’re going to look for deformity."
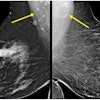
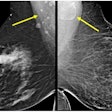
A normal axillary lymph node will appear as an ovoid or elongated fat-filled structure. Most often, the central fat is markedly echogenic, Fornage explained.
But in lymph node metastases, the sonographic sign is decreased echogenicity. As a result, minute early metastatic foci can be found either as a totally echogenic fatty node or as a bulge at the surface of the node.
Lymph nodes that are massively involved with metastatic tumor are recognized on ultrasound as rounded or irregularly shaped masses with little or no residual echogenic fat. These suspicious findings are generally confirmed by ultrasound-guided fine-needle aspiration, Fornage said.
Other areas where ultrasound can be beneficial:
- Local staging in order to determine the true size of a carcinoma, although some cancers, such as invasive lobular carcinoma, are not well defined by sonography.
- Detecting additional foci of carcinoma, particularly in dense breasts. The precise mapping of lesions and the accurate measurement of distance between lesions allows for the differentiation between multifocal disease (multiple foci in the same quadrant within a distance of 3 cm) and multicentric disease (multiple foci more than 3 cm apart or in different quadrants). This is important because most surgeons will not opt for breast-conserving surgery in patients with multicentric tumors, Fornage said.
- Quantifying the response of breast tumors to preoperative chemotherapy by measuring the volume of index lesions before and after treatment. Ultrasound also can be used to guide the placement of metallic markers by the carcinoma that is responding to chemotherapy. This helps the surgeon locate a tumor if it needs to be excised, Fornage said.
However, Fornage cautioned that one pitfall is that benign reactive hyperplasia can mimic metastatic nodules on ultrasound exams. This is especially an issue in elderly patients with rheumatoid arthritis and younger women who are nursing. In both cases, swollen or enlarged lymph nodes should not be mistaken for metastases, he said.
By Shalmali PalAuntMinnie.com staff writer
October 17, 2001
Copyright © 2001 AuntMinnie.com