It's Friday afternoon, the work week is over, and 19 women are waiting for their paychecks. One talks about the pot roast she’s making for a dinner party. Another can’t wait to sleep in Saturday and then take her kids to the park. But after they get their checks and before their weekend begins, they have an appointment at the mobile mammography van right outside.
Their company, based in Valencia, CA, has sponsored a mobile mammography unit. Without it, four of these women would not have been diagnosed with breast cancer in time. They wouldn't now be on the road to recovery without access to convenient mammography screening.
For Catherine Midgette, executive vice president of Mobile On-Site Mammography in Tempe, AZ, the main point is access.
"Ninety percent of women tell me that they would not get a mammogram if it wasn’t right outside their door," Midgette said. "That’s the beauty of the mobile business: you can serve everyone in any type of place."
Patient convenience aside, mobile breast imaging does, from the mammographer's point of view, come with economic and environmental pitfalls. The hardships of making ends meet while making money is an issue that program directors, technologists, and radiologists must contend with.
"There are so many conflicting issues that cause you to get so frustrated," said Midgette, who is also an RT. "You have to constantly live the mission that you are in the business of saving lives, not making money."
Getting started
Mobile mammography startup fees can run anywhere from $100,000 to $500,000, depending on the size of the vehicle and equipment involved. Operating costs for a day of screening range from $2,700 to $3,000. Diesel gasoline prices, hotel, and travel accommodations must also be considered, particularly for out-of-state or remote locations. Midgette’s company frequently travels to California, if a company or person is willing to pay the fees.
Another financial consideration is reimbursement. Insurance providers don’t distinguish a mobile unit from a fixed site, even though the cost of running a mobile unit is two-and-a- half times greater, said Midgette, who’s been doing mobile mammography for 11 years.
"Even though it looks like a cookie cutter situation, it’s not," said Jean Griswold, founder and CEO of Mobile Health Outreach in Charlotte, NC. "We must work in tandem with fixed sites so that we can survive."
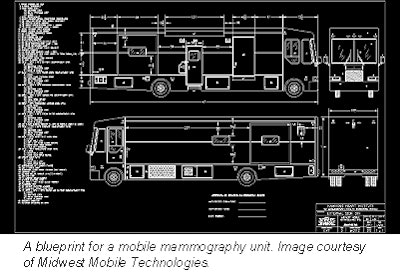 |
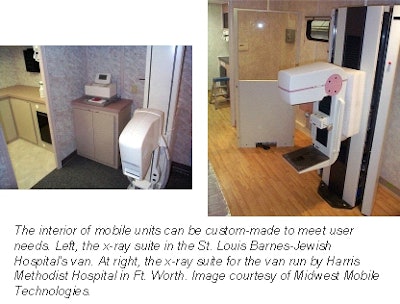
Logistics present another problem onboard the typical 80 feet long vehicles. Only mammography screenings -- not diagnostic tests -- can be conducted. If a diagnostic test is required, the patient will have to visit a fixed location for follow-up -- something a woman may not be willing to do if she is hampered by time and transportation constraints.
"It would be a lot easier for us to go pick up these women and bring them to a site for initial tests and follow-ups," said Roberta Edge, a RT and director of medical imaging at the Kaweah Delta Health Care District Community Breast Center in Vasalia, CA.
Image quality
Unlike a hospital where climate control is a given, mobile mammographers must contend with the elements. During the summer months, heat and humidity must be taken into consideration, while potential freezing temperatures are an issue in winter. Either way, it can take a toll on the technical quirks of imaging processing.
"Processing the film becomes a very difficult situation. Out there in a strange environment, you never know how the equipment is going to react. Dirt is my biggest enemy," said Deb Wright of Valencia Mobile Mammography in Valencia, CA.
Sharon Haworth, chief radiologic technologist at Seattle’s Imaging Associates, agreed. "Luckily, though, the images usually come out as high-quality as those at a fixed site. We have more quality control and assurance loops to jump through, so our images are very comparable to what on-site radiologists are making."
 |
According to the Mammography Quality Standards Act (MQSA), each mobile is subject to inspection, including annual equipment quality control tests.
Reports published on mobile mammography say image quality ranges from good to adequate. In a 1995 study, Dr. Edward Sickles from the University of California, San Francisco, evaluated nearly 67,000 breast exams that had been performed in mobile vans over a 10-year period. One of the issues he looked at was the rate of repeat examination due to poor image quality. According to the results, "no differences were found in the rates at which repeat examination was necessary. Latent image fading is not accompanied by clinically relevant impairment of results (Radiology, February 1995, Vol.194:2, pp. 389-392).
Irish investigators were slightly more cautious in their assessment of mobile film processing. According to their study at the Eccles Street Breast Screening Center in Dublin, "initial quality control (QC) sesitometric tests revealed a large variation in film processor performance in the mobile unit." Using abnormal mammograms done on-site at the center as reference material, the images were matched with QC film density variation from the mobile unit, and ranked for spatial and contrast resolution. While they concluded that with careful monitoring, mobile screening images can be comparable to those done in the hospital, on-site film processing still has the edge (British Journal of Radiology, December 1992, Vol.65:780, pp. 1097-1101).
A small portion of the images might suffer from motion distortion, "but this is such a minor thing," said Dr. Tom Cink of Sioux Valley Hospital in Sioux Falls, SD.
Not everyone is convinced that mobile units are as good as on-site mammography. Meeting MQSA standards is one thing; meeting the reading standards of a radiologist is another, said Dr. Michael Linver, director of mammography at X-Ray Associates of New Mexico in Albuquerque.
"The quality of most mammo images done at mobile sites is almost always inferior to that obtained at fixed sites, but is still generally adequate to pass the fairly stringent requirements for MQSA certification and definitely is adequate for diagnostic purposes," he said. Films that have imperfections due to motion, underexposure, or improper positioning can cause problems for many radiologists.
Self-starters wanted
Other than these unique mobile dilemmas, the units must acquire and train people who are particularly suited for an on-the-go career. Engineers must be certified, technologists must be ARRT mammography certified, and drivers need to have the proper licenses. In addition, a mobile unit must be FDA certified and undergo a physicist survey.
 |
"It can take you a good month to get a program underway," said Griswold. "The best thing to do is to hire self-starters who have a knack at solving problems and making any situation work."
Yet a succession of difficult situations and intense workloads can burn out many employees, Griswold said. Nevertheless, she added, the rewards are so huge for her and many of her colleagues that they outweigh the difficulties of an on-the-road job.
"When you go out into a community that doesn’t know what a mammogram is or how to do a self-examination, you empower a woman to recognize that she is worth something," said Betty Meyer, clinic manager of the Sioux Valley Breast and Bone Health Institute in Sioux Falls, SD. "The appreciation overflows and you can’t help but feel good about what you’re doing."
Many clinic directors and technologists enjoy the sense of teamwork that develops between the mobile programs and community liaisons. The community link helps programs reach people who would not otherwise get mammograms, such as busy corporate workers, minority populations, and transient women.
In these circumstances, mobile units can detect four cancers in 12 days, which Wright’s team found. Or they discover early breast cancer that would turn aggressive and cause death within two years, such as what Midgette’s group discovered. Such an abysmal lack of knowledge exists in these realms that screenings, however they’re done, are necessary, said Griswold.
"Mobile units are a way for us to be proactive in wellness care," said Griswold. "We must plant the seed so that women can care for themselves more. All it takes is 15 minutes. "
Mobile mammo: The way of the future?
On-site mammography units will continue to be the ultimate go-to in breast cancer detection, sources confirm. Mobile units, at least for now, will exist as vital resources for women who are in need of convenient screening opportunities.
Fixed units will continue to win overall because they can find a potential problem on the screening exam and do more testing right then and there, said Dr. Cheryl Viglione, of Southeastern Radiology in Greensboro, NC. But in the battle to get more women screened and aware of breast cancer, mobile units will give fixed sites a run for their money.
"In rural settings or isolated environments, a fixed site can’t exist for economic reasons," Dr. Tom Cink said. "Mobile is the only way women are going to be screened."
Integration of the two sites seems to be the best answer, Haworth said. As in many other industries, though, the quest for dollars or the perpetuation of the status quo can stall beneficial programs from reaching the public, said Midgette. "If we are to be about the patient and her health, both units will be vital for everyone’s success."
By Krystina SibleyAuntMinnie.com contributing writer
August 23, 2001
Copyright © 2001 AuntMinnie.com