More than 470 million women worldwide are over age 50, according to the North American Menopause Society, and it's a safe bet that many of them are already on hormone replacement therapy (HRT). For imaging specialists, HRT can pose dilemmas ranging from changes in breast density to confusing enhancement patterns. Two recent studies looked at HRT's effects on screening mammography, as well as on MR exams.
While working at the University of Lund in Malmo, Sweden, Dr. Caroline Blane investigated increasing breast density in screening mammography. Blane is a professor in the radiology department at the University of Michigan in Ann Arbor. She presented the results of her work at the 2001 American Roentgen Ray Society meeting in Seattle.
"One of the reasons that mammography is a successful screening test is the low cost of the test," Blane said. "This low cost is related to the relative ease of interpretation of the study. The increasing fatty content of the breasts with aging contributes to this ease of interpretation. Screening for breast cancer in the dense breast is more time-consuming than one with considerable fat. So any overall significant change in the proportions of fat to fibroglandular tissue in the breasts has a direct influence on screening mammography."
Assessing whether HRT has any effect on these changes in breast density as well as fatty tissue was one of goals of the study, she said.
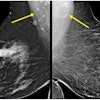
For this prospective analysis begun in December 1996, mammography studies from 261 consecutive breast cancer screening patients were compared with images obtained five years earlier. The studies were quantified for degree of breast tissue density using BI-RADS criteria, with 4 representing an extremely dense breast and 1 a completely fatty breast. The patients ranged in age from 50 to 59 years. The radiologic technologist obtained the HRT status of the patients.
"Then, from the University of Lund archives, 261 age-matched patients who had mammograms 10 years earlier in 1986 were located and then were coded for breast density. Each of these patients had a mammogram [in 1981] and this was coded for breast density," Blane said. "HRT is relatively new in Sweden. Looking at the screening population in 1996, less than .004% were on HRT for more than 10 years. It is unlikely that those in the case group of 1986 were on HRT."
Analysis of variance was used to determine differences between the control group, the group on HRT, and the group not on HRT.
According to the results, the mean breast density in 1991 (2.26) did not differ from the 1981 mean of 2.21. However, there was a statistically significant decrease in breast density between initial mammogram screening in 1981 and the second one in 1986, indicating that "breasts in the ‘80s were becoming more fatty," Blane said.
The patients from 1996 were divided into three groups: a control, those on HRT and those who were not. The change -- toward lower breast density -- over the five-year interval in the control group was significantly different from that of the HRT group and the group without HRT (p<.05).
"We then looked at several of the variables to determine the effect of HRT," Blane said. "If you look at the 1996 mammograms, they were denser than the 1986 ones, irrespective of whether the patients were on HRT or not. We also looked at the length of time on HRT and we could not find any effect. There are clearly more important influences on the rate of change in breast density than HRT." Other factors that may play a greater role in increasing breast density are parity, weight, and age at first birth, Blane suggested.
"The importance of this observation is that increasing breast density renders the screening test more difficult and time-consuming," she concluded. "Denser mammograms have been shown to be associated with increased false positive biopsy rates. However, HRT is only one variable in these changes."
MRI and progesterone-based HRT
Medications containing progesterone gave researchers at the University of Bonn in Germany the greatest trouble when it came to contrast-enhanced MR imaging of post-menopausal women on (HRT).
In a prospective intra- and interindividual comparative study of 62 healthy volunteers, Dr. Christiane Kuhl and her colleagues looked at the effects of HRT on contrast enhancement in breast MRI.
"The questions we asked were: Are there contrast enhancement areas that are clearly attributable to HRT? How often do contrast-enhancing areas arise? If they do arise, do they pose any differential diagnosis problems and do they interfere with the early detection of possible breast cancer?," Kuhl said in a presentation at the 2000 RSNA conference in Chicago. "Finally, how long does it take for contrast enhancement uptake to return to normal values after discontinuation of HRT?"
All of the women in the study underwent three breast MRI studies every four to six weeks. They were then assigned to three groups: Group A consisted of 15 premenopausal women, group B was made up of 20 postmenopausal women who were not receiving HRT, and group C consisted of 27 age-matched, postmenopausal volunteers who were on HRT.
"After the second MRI study, group C was asked to discontinue HRT. That way, we could compare the effects of endogenous hormones with the effects of exogenous hormones. We also could intraindividually compare the effect of exogenous hormones compared to baseline," Kuhl said.
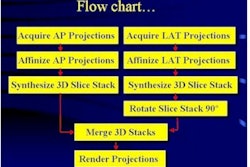
Standard dynamic, contrast-enhanced subtraction breast MR was performed using a bilateral coil (1.5T ACS II, Philips Medical Systems, Shelton, CT). Twenty-one sections were acquired with 4-mm thickness, a field-of-view of 300 mm and a full 256 x 256 imaging matrix.
Two blinded readers evaluated the images for the following: presence and degree of parenchymal enhancement, prevalence of focal contrast-enhancing areas, and an overall impression by rating the studies as clearly benign, equivocal, or suspicious.
Parenchymal enhancement of group C was significantly stronger than with group B, Kuhl reported, although group C’s results were comparable with group A. After discontinuing HRT for four to six weeks, group C’s levels were reduced to match group B’s.
Prevalence of focal contrast-enhancing areas was 65% for group C, 33% for group B, and 75% for group A. The prevalence of focal lesions with significant enhancement was highest in group C at 83%, compared to group B at 35% and group A at 47%.
Finally, "when the readers were asked whether or not the lesions they had seen were suspicious, the women on HRT (group C) had the highest number of lesions that were rated suspicious," Kuhl said. This was particularly true of the patients with progesterone-containing HRT.
Readers rated 56% of the images in group C as clearly benign, compared to 95% in group B and 71% in group A. Once again, after discontinuing HRT for as long as six weeks, the prevalence of lesions with significant enhancement decreased in group C so that 92% of the studies were read as clearly benign.
Kuhl recommended that healthcare professionals ask patients who are undergoing HRT therapy to stop their regimen before MR imaging.
By Shalmali PalAuntMinnie.com staff writer
June 11, 2001
Related Reading
Increased breast density reverses after discontinuation of HRT, January 11, 2001
Women receiving HRT not likelier to need second mammogram, April 29, 2000
Click here to post your comments about this story. Please include the headline of the article in your message.
Copyright © 2001 AuntMinnie.com