NEW ORLEANS - Despite the vast array of treatments available for patients with cardiovascular disease, doctors are still puzzled by "residual risk" -- patients who fall through the cracks and have unrecognized cardiac risks.
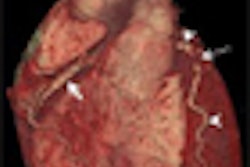
Researchers are coming to believe that even the best biomarkers, such as C-reactive protein and cholesterol levels, and the Framingham risk score may be inferior to imaging techniques such as ultrasound carotid intima-media thickness measurements, CT coronary artery calcium scans, and vascular function measurements. The evidence suggests that such methods have greater predictive value for adverse events than traditional risk assessment techniques.
At a symposium sponsored by the Society for Heart Attack Prevention and Eradication (SHAPE) during the American Heart Association (AHA) Scientific Sessions 2008, speakers reviewed data on various methods of predicting cardiac events.
"Most heart attacks occur in persons misclassified as low risk," said Dr. Erling Falk, Ph.D., a professor of medicine at Aarhus University Hospital in Skejby, Denmark. "Most persons at high risk are also misclassified," he said, based on data from the Women's Health Study. Dr. Falk noted that 99 of the 199 events occurred among the 6,944 women with "low risk" indicators, and that even among women classified as high risk, events occurred in just 19 of 59 of these individuals.
In the Northwick Park Heart Study, which utilized the predictive values of C-reactive protein and the Framingham score, 140 of 159 events occurred in the lowest-risk group. Just 19 of 84 persons deemed high-risk had events.
In another presentation at the symposium, Dr. Matthew Budoff, an associate professor of medicine at Harbor-UCLA Medical Center in Torrance, CA, said that electron-beam CT showed better predictive value than the Framingham score. In fact, he cited studies showing the superiority of calcium scores in predicting outcomes. Patients who achieved a calcium score of 0 had no cardiac events after 2.3 years of follow-up, he said.
Carotid intima-media thickness measurement progression that can be performed with increasingly sensitive ultrasound devices also gives doctors a better idea of who is at risk of cardiac events, said Dr. Allen Taylor, a professor of medicine and chief of the cardiology service at Walter Reed Army Medical Center in Washington, DC.
"Intima-media thickness changes as a biomarker has a broad track record of success," he said. "Changes in intima-media thickness are definitely linked to clinical outcomes."
The findings of adverse change in thickness permit clinicians to treat patients with a broad range of therapeutic options, he said.
Endothelial function testing, an emerging new field for predicting patient outcomes, also adds to other risk scores to give a better idea of what the future holds for patients, suggested Dr. Amir Lerman, a professor of medicine at the Mayo Clinic in Rochester, MN.
He noted that endothelial function testing is more than 20 years old, and scientists have shown that endothelial function is related to strokes, sleep apnea, dementia, myocardial infarction and sudden death, renal failure, claudication, erectile dysfunction, and the metabolic syndrome.
Studies show that combining endothelial function tests and the Framingham risk score improves the predictive value of cardiac events, Lerman said.
By Edward Susman
AuntMinnie.com contributing writer
November 12, 2008
Related Reading
ACRIN study: Cardiac CTA cheaper, more effective for chest pain triage, October 14, 2008
Anemia, CKD predict presence and severity of coronary artery disease, September 22, 2008
Echocardiography method predicts CAD, September 16, 2008
Quantitative stress echo can reliably find coronary artery disease, August 18, 2008
MRI evaluation of chest pain cuts acute coronary syndrome, August 15, 2008
Copyright © 2008 AuntMinnie.com