BERLIN - Automated tracking methods, used to guide biopsy needles, imaging probes, and ablation devices into patients during interventional radiology procedures, have come a long way in a few short years. And they still have a long way to go.
But where investigators in the past might have been happy to see a robotic needle arm move across a lab table, they are now privy to seeing real patients getting punctured -- accurately -- based on the calculations of such automated systems.
Among the more important studies unveiled at the opening of the 2007 Computer Assisted Radiology and Surgery (CARS) conference on Wednesday was a project led by Philips Medical Research North America of Briarcliff Manor, NY, in cooperation with the Intramural Research Program of the National Institutes of Health in Bethesda, MD; Traxtal of Toronto; and NDI of Waterloo, Ontario.
"Electromagnetic tracking has been demonstrated for real-time ultrasound and CT fusion and navigation on preacquired images in laboratory studies, animal studies, and clinical trials of older tracking equipment," said Dr. Jochen Krücker of Philips Medical Research. The aim of the present study was to build a highly accurate tracking system and use it in patients, he said.
Navigation systems are invaluable for minimally invasive interventional procedures because they can spatially track preacquired and preoperative images, and track interventional devices such as needles with the aid of miniaturized electromagnetic devices attached to the tip.
The payoff in terms of more successful procedures and fewer complications is potentially immense, and with better tracking, healthcare costs could be reduced significantly as well. All this has spurred great interest in refining the systems and getting them into interventional radiology suites, where most tracking, positioning, and aiming is still the result of an educated guess by interventionalists who examine a few preprocedural images and maybe place a few skin markers.
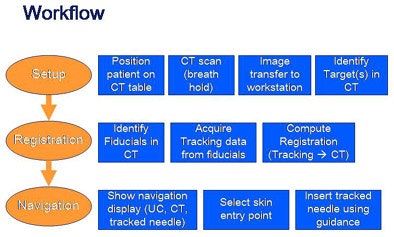
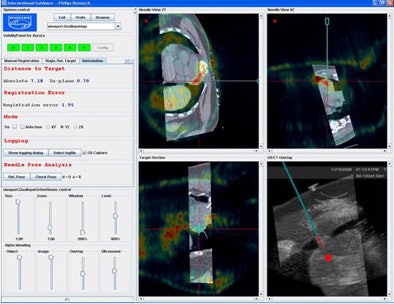
Krücker and his colleagues built and tested a prototype interventional navigation system to evaluate electromagnetic tracking during soft-tissue ablation and biopsies.
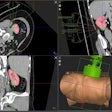
The system was based on the 2005 Aurora "square" tracking system (NDI) along with several additions, including custom Philips software that enabled tracking of a needle, an ultrasound probe (iU22 scanner, Philips Medical Systems, Andover, MA), and up to eight respiratory motion sensors relative to 3D images (Traxtal). The system supports manual registration and simultaneous display of two 3D images.
An electromagnetic tracking sensor was attached to the ultrasound probe and guided by customized stylus/sheath combinations and tracked radiofrequency ablation needle guides with integrated miniaturized sensor coils in the needle tip (Traxtal). The accuracy of needle tracking was compared with the needle position at CT.
"For analysis we compared the confirmed position with the fiducials with several confirmation CT scans," he said. Also, targets were compared based on conventional ultrasound or 16-detector-row CT guidance (Brilliance, Philips Medical Systems).
 |
| All charts and images courtesy of J. Krücker, S. Xu, N. Glossop, Z. Neeman, J. Locklin, and B.J. Wood. |
The tracking analysis was performed on 18 patients (13 men, 5 women; mean age 58.4 ± 12.9 years) in order to perform 11 radiofrequency ablations and seven biopsies in target sites that included the liver (11), kidney (3), lung (2), neck (1), and above the heart (1).
"A nice example of why tracking is so attractive for these procedures is because needles can and do bend," Krücker said. Calculating needle position based on the insertion angle can result in significant errors, and the study results included needle angle insertion tracking in six of the patients compared to conventional image guidance.
"The procedures were all clinically successful; we had a total of 41 confirmed needle positions in those 18 patients (one to four per patient)," Krücker said. "The average fiducial registration error was 1.5 mm, and the additional setup time, the steps that were necessary for the procedure compared to conventional workflow, was about six and a quarter minutes using the passive fiducials only."
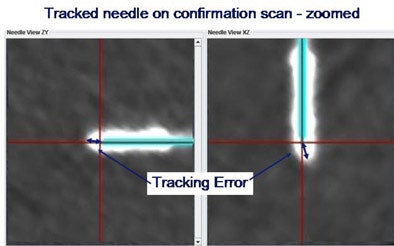 |
Compared to traditional CT or ultrasound guidance, the average tracking accuracy of the system was 3.8 mm when using only external skin fiducials for registration, improving to an average of 2.9 mm when an internal needle position was also used for registration.
Finally, the researchers compared the results of different aiming methods with the tracking system versus conventional ultrasound/CT guidance. That is, two interventional radiologists did their best to aim the needles based on viewing CT/ultrasound images, versus aiming with the tracking system.
 |
| Above, tracking angle for radiofrequency ablation of the lung based on CT/ultrasound guidance versus tracking method (below) yielded better results with automated tracking. |
 |
Based on eight data points in six patients, and with a mean distance from the target of 78 ± 33 mm, the in-plane distance was 2.4 mm ± 1.2 mm with navigation compared to 14.4 mm ± 7.4 with conventional CT/US, and the difference in angles between the two methods was 10.5° ± 2.8°, Krücker said.
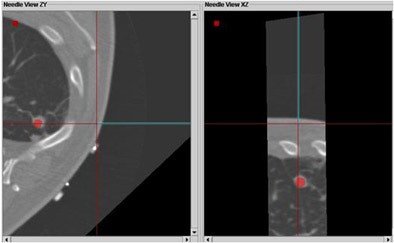
In two cases the researchers also successfully registered preprocedural CT scans with prior DICOM images. Registration with a prior MR scan was used for a renal radiofrequency ablation, and registration with a prior PET/CT scan was used to biopsy a lymphoma close to the heart, an organ that is critical to avoid during such procedures.
 |
| Registration with a prior PET/CT scan was used to biopsy a lymphoma close to the heart. |
The results showed that the tracking system is accurate in the CT interventional suite with internal errors of around 3.8 mm, and the internal needle improves accuracy further to within 2.9 mm, Krücker said. The system improves needle aiming significantly as well, and provides target position information that would otherwise be unavailable, compared to only CT- or ultrasound-guided procedures, he said.
Future work will include motion compensation, incorporating active external and internal fiducials, and a multicenter trial to show the clinical benefits of the system, Krücker said. Multimodality registration with the tracking system is easy and accurate.
Compensating for the highly variable motion produced by breathing, heartbeat, and patient movement is one of the major challenges facing researchers today, he noted.
By Eric Barnes
AuntMinnie.com staff writer
June 28, 2007
Related Reading
Electromagnetic navigation aids bronchoscopy biopsy of peripheral lesions, June 13, 2007
Part III: Image processing has room to grow, October 23, 2006
Part II: Medical image processing has room to grow, September 4, 2006
Part I: Medical image processing has room to grow, July 4, 2006
Copyright © 2007 AuntMinnie.com