Lymphomatoid Granulomatosis:
Angiocentric lymphoma or Angiocentric immunoproliferative lesion
Clinical:
Lymphomatoid granulomatosis has recently been termed- angiocentric immunoproliferative lesion (AIL). It is a rare form of non-Hodgkins lymphoma [8] with an angiodestructive lymphoreticular and granulomatous disease with a prediclection for extranodal involvement- most commonly the lungs. There is a oligoclonal or monoclonal proliferation of CD20-positive B-cells (some of which are infected with EBV) among a background of polyclonal reactive CD3-positive T-cells [7]. The lymphoid infiltrate surrounds muscular arteries and veins early in the disease course, and typically invades the walls of the vessels which results in vascular compromise and infarction.
The majority of affected patients are middle aged (40-60) and present with fever, cough, hemoptysis, malaise, rash, and weight loss. The disorder is more common among immunocompromised patients and affects males twice as often as females [6]. The lungs are the most commonly involved site [6]. Skin lesions (ulcers, subcutaneous nodules, or maculopapular eruptions) are found in up to 40-50% of cases (the most frequent site of extra-pulmonary disease), and CNS involvement occurs in 20-30% (peripheral neuropathy, cranial nerve palsey, or mass lesion). Skin lesions occur prior to chest radiologic abnormalities in up to one-third of patients. Unlike Wegener's, involvement of the paranasal sinuses and kidneys are not typical features of the disease, although they can be affected. The disease typically has a rapid onset and progression- mortality approaches 60%, particularly in patients with CNS or liver involvement (CNS involvement is associated with a poor prognosis [7]). An association with the Ebstein Barr (E-B) virus has been described- most cases of AIL represent a proliferation of E-B virus infected B-cells with a prominent T-cell reaction and vasculitis [4].
Diagnosis usually requires open lung biopsy as transbronchial biopsy is positive in only about 30% of cases. The disordered is graded based upon the degree of cytologic atypia from Grade I (little or no atypia) to Grade 3 (prominent atypia- angiocentric lymphoma). About one-third of patients with grade I lesions progress to malignant lymphoma, while nearly two-thirds of patients with grade 2 lesions will develop lymphoma (look for presence of mediastinal/ hilar adenopathy to suggest the development of lymphoma). Combination cytotoxic therapy is the treatment of choice, but is generally unsuccessful. Overall prognosis is poor and most patients do not survive more than 2 years [5] (the 5 year mortality os 60-90% [6]).
X-ray:
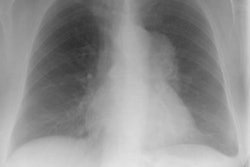
The CXR appearance is similar to Wegener's granulomatosis- bilateral lung nodules ranging in size from 1 to 5 cm are found in up to 70-80% of cases. Most nodules are smaller than 1 cm and predominate in the middle and lower lung zones [6]. The borders of the nodules may be poorly defined or sharp [6]. The nodules are typically distributed along the bronchovascular bundles or interlobular septa [6]. Cavitation occurs in about 20-25% of nodules. Findings are bilateral in 90% of cases.
Diffuse, coarse, reticulonodular infiltrates may also be seen less commonly (4 to 40%). Adenopathy is rare in the absence of lymphoma. Pleural effusions are uncommon and if present suggest pleural involvement (although other authors describe the presence of effusions in up to 30% of cases [5]).
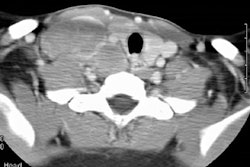
On CT, the findings include the presence of multiple well or
poorly defined nodules (5 to more than 60) generally less than 1
cm in size (but up to 6 cm) [4]. The nodules have a peribronchovascular distribution and
small nodules can coalesce to form larger conglomerations [4].
The lesions may contain air bronchograms and a peripheral
ground-glass halo [7]. Thin walled cysts (1-2 cm) can be seen in
up to 60% of cases [4].
Mediastinal lymph node enlargement is rare [7]. Pleural
effusion is sometimes present [7].
The lesions are FDG avid [7].
REFERENCES:
(1) Radiol Clin North Am 1991 Sep;29(5):973-982
(2) South Med J 1995 Jul;88(7):771-775
(3) Mayo Clin Proc 1990; 65:151-163
(4) AJR 2000; Lee JS, et al. Lymphomatoid granulomatosis: Radiologic features and pathologic correlations. 175: 1335-1339
(5) Radiographics 2002; Gimenez A, et al. Unusual primary lung tumors: a radiologic-pathologic overview. 22: 601-619
(6) Radiology 2011; Rezai P, et
al. Lymphomatoid granulomatosis. 259: 604-609
(7) Radiographics 2016; Sirajuddin A, et al. Primary pulmonary
lymphoid lesions: radiologic and pathologic findings. 36: 53-70
(8) Radiographics 2020; Naeem M, et al. Noninfectious granulomatous diseases of the chest. 40: 1003-1019