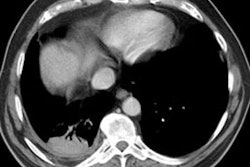
Silo Filler's Disease (Nitrogen Dioxide Inhalation):
Clinical:
The disorder occurs secondary to nitrogen dioxide exposure. Silo filler's disease is also seen in arc welders, following rocket fuel exposure, and following exposure to burning nitrogen waste. The disease is characterized by 3 phases:
1- Acute phase: Develops within 2 to 4 hours of exposure and represents a chemical pneumonitis. There is diffuse alveolar wall damage with pulmonary edema.
2- Latent phase: This phase lasts 2 to 4 weeks and represents a period of biological repair.
3- Bronchiolitis obliterans phase: The reparative process actually results in destruction of terminal bronchioles.
X-ray:
On plain film a pattern of pulmonary edema is identified in the acute stages of the disorder. Later, there are nodular densities, atelectasis, and obstructive emphysema.