Healthcare information technology produces tangible benefits in terms of fewer patient complications, lower mortality rates, and lower costs, according to a new study published this week by researchers from Johns Hopkins University in Baltimore. For every 1,000 patients, five fewer will die at hospitals that have the highest levels of computerization, according to the researchers.
Hopkins researchers conducted a large cross-sectional study comparing levels of use of clinical information technologies such as electronic automated notes and records, computerized physician order entry, and clinical decision support software. They found that hospitals using healthcare IT tools delivered better, more cost-effective care for patients with myocardial infarctions, congestive heart failure, coronary artery bypass grafting, and pneumonia.
The study evaluated the records of 167,233 patients treated at 41 hospitals located in urban cities throughout Texas. It was published in the January 26 issue of the Archives of Internal Medicine (January 2009, Vol. 169:2, pp. 108-114).
Healthcare IT advocates have long speculated that clinical information technologies would improve clinical and financial outcomes. But few studies have analyzed this relationship in a large number of hospitals, according to the study's lead author, Dr. Neil Powe, director of Johns Hopkins' Welch Center for Prevention, Epidemiology, and Clinical Research.
Hopkins researchers selected the state of Texas for the study because it contains a large and diverse patient population and a wide range of hospitals for which specific clinical outcomes could be obtained. Seventy-two general acute care hospitals located within 10 geographically dispersed metropolitan areas were identified.
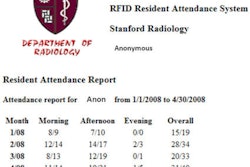
The researchers used the Clinical Information Technology Assessment Tool (CITAT), a questionnaire administered to physicians who provide inpatient care, to assess the degree to which clinical information processes in a hospital are computerized. The questionnaire measures a hospital's level of automation based on a physician's daily interaction with various healthcare information systems.
The CITAT survey was mailed between December 1, 2005, and May 30, 2006, to 7,432 physicians, representing a 50% random sample of family practice, internal medicine, or general surgery physicians in Texas. The survey divided hospital automation into four categories, including test results, notes and records, order entry, and decision support.
For each category, physicians were asked if an electronic system was implemented in the hospital, whether they knew how to use it, and whether they used it consistently. For a hospital to be included in the study, a minimum of five physicians had to identify it as the primary hospital for inpatient admission of the physician's patients. A total of 41 hospitals qualified.
The researchers then evaluated inpatient mortality, complications, costs, and length of stay among patients 50 years and older who were admitted to all 72 hospitals during the survey period to be treated for myocardial infarction, congestive heart failure, coronary artery bypass grafting, and pneumonia. These conditions were selected for evaluation because the researchers believed that the illnesses were sensitive to clinical guidelines and representative of reasons for hospital admission.
For each hospital, statistics were obtained for type of ownership, bed size, and total margin. Estimates of the risks of complication and mortality for each hospitalization were obtained from the risk-adjusted complication index and risk-adjusted mortality index variables provided in each hospital's claims data field. The hospital characteristics and CITAT scores were linked by hospital to the discharge data.
The 41 hospitals with healthcare IT technology tended to be larger, with an average of 402 beds, compared with 216 beds at the 31 hospitals that did not have computerization. Six of the 41 hospitals in the cohort were academic teaching hospitals. The 41 hospitals also documented shorter lengths of stay. There were no statistically significant differences with respect to hospital mortality rate, complication rate, median costs, type of ownership, operating margin, total margin, or information technology operating expenses.
Major findings of the study included the following:
- Hospitals with higher automation scores for all four categories were associated with a statistically significant decrease in the adjusted odds of inpatient mortality for pneumonia, myocardial infarction, and coronary artery bypass graft procedures.
- Each 10-point increase in the score of computerized automation of notes and records was associated with a 15% decrease in inpatient mortality for all causes, as well as reductions in risk of mortality for each disease admission category.
- There were fewer patient complications at hospitals with higher automation scores. Hospitals with the highest scores for utilizing computerized clinical information systems were associated with a 21% decrease in the odds that a patient would develop complications.
- Hospitals with the highest levels of computerization recorded five fewer deaths for every 1,000 patients.
However, hospitals with higher scores for use of electronic medical records and notes had higher scores for complications associated with heart failure. The authors suggested that this statistic may result from electronic documentation recording adverse events more accurately and with greater detail and, therefore, capturing this data better than hospitals with lower scores.
- Higher scores on decision support, order entry, and tests results were overwhelmingly associated with lower mean hospital costs for all patient admissions. The test results category included laboratory information systems, radiology information systems, and PACS, which represented the largest type of healthcare information systems adopted by the 42 hospitals.
- There was no statistically significant difference between level of healthcare IT utilization and length of patient stay.
- There was no relationship between the degree to which physicians' orders were computerized and the rate of complications.
- Greater automation of test results was not associated with a lower risk of hospital death or complications. The authors suggested that a minimal level of automation may be sufficient to protect patients and is already in place at most of the hospitals in the study.
The authors believe that their study proves that for certain conditions, greater automation of a hospital's information system may be associated with reductions in mortality, complications, and cost. Furthermore, healthcare information systems designed around clinical workflows can contribute to improving healthcare outcomes and reducing costs in hospitals that deploy them.
By Cynthia E. Keen
AuntMinnie.com staff writer
January 27, 2009
Copyright © 2009 AuntMinnie.com