SAN ANTONIO - As the front-end of a PACS network, image displays are key factors in the success of digital image management. PACS purchasers have much to consider when deciding on image displays: hardware, software, quality assurance, and even location must be weighed, said Katherine Andriole, Ph.D., PACS clinical coordinator at the University of California, San Francisco.
Andriole detailed these considerations during a presentation Thursday at the PACS 2003: Integrating the Healthcare Enterprise conference, being held this week in San Antonio.
On the hardware front, users must decide whether to go with 2K or 1K monitors. The American College of Radiology still recommends 2K displays for primary diagnosis of computed radiography exams and digitized films, Andriole said.
However, many radiologists have become comfortable reading and providing primary diagnosis of these studies from much less expensive and longer-lasting 1K displays, taking advantage of zoom and pan functions to instantly access full-resolution data as needed, she said. The 1K displays are definitely acceptable for the lower-resolution cross-sectional modalities.
The decision to go with portrait or landscape models is a toss-up, and depends on personal preference, she said. As for the number of monitors needed, Andriole said that two-headed displays are suitable to meet diagnostic needs.
"The monstrosity of four or eight monitors is not necessary and not cost-effective," she said.
The dual-headed configuration is needed in many cases to compare current and prior studies, particularly for projection radiography exams, she said. A robust graphical user interface (GUI) can reduce the need for multiple monitors if it includes functionality such as image movement/paging, switching between tile and stack modes, side-by-side comparison on one monitor, and multiple studies per monitor, she said.
The type of monitor -- traditional cathode ray tubes (CRT) or flat-panel displays -- is also an important consideration. Liquid crystal displays (LCD) have a number of advantages over CRT models, including higher luminance and less drift, a longer lifetime, small pixel sizes, and reduced reflection and sensitivity to ambient room lighting, Andriole said.
On the other hand, some LCDs may be subject to off-angle viewing problems, in which viewers may see a different image quality based on their viewing angle to the display, she said. In addition, flat-panels are typically more expensive than CRTs.
The monitor luminance affects perceived contrast resolution as well as perceived spatial resolution, Andriole said. And many studies have concluded that diagnostic accuracy improves as the luminance increases.
This issue is particularly relevant in the complex decision of color versus monochrome displays. Color yields decreased luminance, contrast, and spatial resolution, and is not optimal for viewing grayscale images, she said. However, color is being used more often now in medical imaging, such as in ultrasound and nuclear medicine, while the emergence of 3-D may require color capability in the future.
Also, high-performance monochrome monitors are currently much more expensive than color displays and have a lifetime of approximately three years, less than color units. On the other hand, the human visual system has decreased spatial resolution, or the ability to pick up fine detail, in the color channels, she said.
As a cautionary note, Andriole cited a recent study from the University of Arizona Health Sciences Center in Tucson, which compared P45 and P104 monochrome displays and color 1600 x 1200-pixel monitors in the detection of pulmonary nodules.
The P45 model, which had decreased grain size and therefore increased signal-to-noise ratio, was superior in overall detection to the P104 display. Both the P45 and P104 displays performed better than the color display (Academic Radiology, June 2002, Vol. 9:6, pp. 638-645).
The color display also produced significantly higher false-positive and false-negative findings, as well as longer search times compared with the monochrome monitors.
"So this is a little bit concerning if you're thinking about color," she said. "On the other hand, we do see color becoming more and more important in medical images."
Software
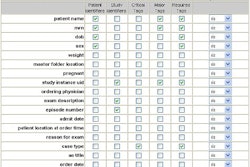
Image display software should include an intuitive GUI, patient lists, an image display component, tools, and be interfaced with the radiology information system and hospital information system, Andriole said.
Different users have different image display needs, which vary by function, modality, and type of examination, she said.
"If you have a user interface that is very flexible and configurable, you can have a wonderful interface for a variety of users," she said.
The software must be fast, robust, and reliable. In addition, it should be able to generate worklists and hanging protocols customized by the exam and for the way each user works, she said.
"Imaging is not just radiology," she said. "What about the folks outside of radiology? They have a lot of special needs. (Orthopedic specialists) need to do measurements, and other physicians need to be able to do this as easily as it was done with film."
Image manipulation functions should include real-time window/level, window and level presets (particularly for CT studies), side-by-side study comparison, and tile and stack (cine) modes. Magnification, as well as zoom and pan features, should be included, she said.
New features showing up on display software include specialty tools such as region of interest (ROI) measurements, 3-D, and computer-aided detection (CAD). The software should also be able to access RIS/HIS information and reports, and determine what prior studies are available on PACS and on film, she said.
Users should also be able to create a summary series, as some clinicians prefer to see only key images. Speech recognition is also increasingly being used, she said.
Displays used to provide Web-based access to images should allow functionality such as window/level, brightness adjustments, and for multiple studies to be reviewed per monitor, Andriole said.
Quality assurance
Once monitors have been installed, they must receive regular quality assurance. Andriole recommends monthly luminance calibration and matching. Some vendors have come out with remote monitoring of monitor statistics.
"I'm hoping that more and more companies will come out with tools that will enable us to do this (monitoring) remotely and automatically," she said.
In other quality assurance tasks, spare parts such as monitors, video cards, and cables should be kept onsite, she said.
"If you have (the spare parts) onsite, you're really never down," she said. "You just swap them out and you're ready to go."
The Society of Motion Picture and Television Engineers (SMPTE) test pattern can also be useful to determine measure drift or the existence of any artifacts. In dual-headed displays, the brightness and contrast for each display should be matched, she said.
The DICOM 14 grayscale standard display function recommends perceptually linearized display function for radiographic images. This is matched to the perceptual capabilities of the human visual system, Andriole said.
If possible, the softcopy reading environment should have low ambient lighting, with the monitor positioned to avoid reflection. The monitors should have an adjustable viewing height, and as much as possible, an ergonomic arrangement of the mouse and keyboard, she said.
Hurdles
Some current hurdles for displays include how the data is presented, Andriole said. Ideally, hanging protocols should automatically be based on the type of examination and the individual viewing the study, with default views and context-based tools.
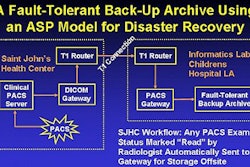
Consistency of display from viewer to viewer, as well as from softcopy to hardcopy, remains a hurdle, she said. This problem is being addressed by the DICOM Committee and within the Integrating the Healthcare Enterprise (IHE) initiative, she said.
Users should also be able to drill down through the database, and be able to access other relevant patient data from within an application, Andriole said. This should be able to be accomplished from one user interface without having to log into the various systems, she said.
In another existing display hurdle, the DICOM standard does not currently include an SQL relational database component. As a result, most vendors implement their own client-server databases within the PACS. With a lot of workstation functionality typically tied to the vendor's core components and database, this can cause problems when mixing and matching displays, she said.
"You need to think about that when you're looking at displays," she said.
By Erik L. RidleyAuntMinnie.com staff writer
March 14, 2003
Related Reading
Medical imaging workstations: What you need to know, May 22, 2002
Digital departments need rigorous QA program, May 5, 2002
Monitor choice impacts diagnostic accuracy and throughput, May 4, 2002
Monitor firms pursue automatic display calibration, May 4, 2002
Radiology workstations need integration, automation, March 15, 2002
Copyright © 2003 AuntMinnie.com