VIENNA - Longer-term results are starting to roll in from radiologists’ use of tumor ablation in the liver, and the results are promising. In particular, a study that aims laser beams at metastatic colorectal cancer lesions may help patients live longer.
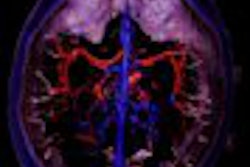
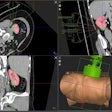
At the interventional radiology sessions of the European Congress of Radiology on Friday, Dr. Martin Mack and colleagues from the J. W. Goethe University in Frankfurt discussed the treatment and follow-up of patients using a teflon-coated, irrigated laser-induced interstitial thermotherapy (LITT ) system (Somatex, Berlin). The intraoperative system has a double-tube protective catheter, and transmits laser light to tumors through flexible fibers, Mack said. MRI guides the procedure and follow-up evaluation.
The group has treated more than 1,200 patients so far, ablating more than 3,400 lesions. Of this number, 702 patients with a total of 2,088 colorectal liver metastases have undergone treatment and long-term follow-up, yielding a wealth of data, Mack said.
"We are always able to introduce significant coagulative necrosis (up to 5 cm). MR shows (both) the size of the initial tumor volume, and the size of the coagulative necrosis, which always exceeds initial tumor volume significantly," he said. "Due to a shrinking effect over time, you see a fall-off at six to 12 months, again a decreasing volume of necrosis."
Initial tumor volumes are fairly evenly divided between 1-5 cm; 29% of patients in the five-year study had tumors of 2-3 cm in diameter, for example.
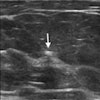
Patients underwent T1-weighted sagittal MRI both pre-and post-treatment, and at repeated follow-up exams. In MR imaging immediately following the procedure, "thermosensitivity weighting produces an increase in T1 relaxation times, and therefore a decrease in signal intensity," he said. The post-procedure images typically show a hypoechoic area of necrosis surrounded by edema.
According to follow-up results, recurrence was very low for all tumor sizes. At six months, 1.8% for tumors up to 2 cm; 2.5% for metastases between 2 and 5 cm in diameter; and 4.3% for lesions 4 cm and larger, he said.
Calculating from the date of lesion diagnosis, the mean survival was 4.3 years for all treated patients (with a 95% confidence interval, 4 to 4.6 years), Mack said. One-year survival was 93%, two-year survival was 75%, three-year survival was 54%, and five-year survival was 23%.
Calculated after the first LITT treatment, mean overall survival fell to 3.7 years. Often patients had chemotherapy after the lesion was diagnosed and before it was treated with LITT, or for other reasons it took a couple of months to make the decision to treat, Mack said.
Survival rates are comparable to those seen in surgical resection, but a wider ranger of patients can tolerate LITT treatment, according to Mack. LITT is especially useful in metastases that are considered unresectable or undetectable, and in patients who refuse to undergo resection, he said.
By Eric BarnesAuntMinnie.com staff writer
March 7, 2003
Related Reading
View from the president: Dr. Nicholas Gourtsoyiannis looks at ECR 2003, March 6, 2003
Radio-frequency ablation effective for many renal cell carcinomas, January 29, 2003
Radiofrequency appears superior to cryosurgery in preventing liver metastases, January 3, 2003
Intraoperative RFA has advantages over percutaneous technique, May 9, 2002
Copyright © 2003 AuntMinnie.com