223Ra-dichloride (Xofigo)
- Clinical:
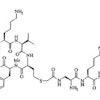
223Ra-dichloride (223RaCl2) is an alpha (α) emitting bone seeking calcium mimetic that forms complexes with hydroxyapatite and will accumulate in areas of increased bone turnover/active mineralization without significant redistribution of the daughter radionuclides [1,2]. The agent is prepared from a long-lived 227Ac/227Th generator [1]. 223Ra has a physical half life of 11.4 days [1] and has a complex decay scheme into 207Pb, a stable daughter nuclide (93.5% α emission, < 3.6% beta-particles, and <1.1% as gamma radiation) [4,5,16]. There are four α particles (5.0-7.5 MeV) generated during each decay with a median penetration range in soft tissue of 0.04-0.05 mm), resulting in high energy deposition (28.2 MeV) and 95% of the energy is from the α emissions [1,16].
Alpha particles are monoenergenic positively charged helium nuclei (initial kinetic energy between 5-9 MeV) that are about 8000 times larger than beta particles [7,9]. Alpha emitters are 100 to 500 fold more potent than low-LET beta-particle emitters [2] and can produce 2000-7000 ion pairs per micrometer in water (one ionization every 2 nm) [11]. Because the diameter of the DNA double-helix is about 2 nm, the traversal of a single alpha-particle is enough to induce double-stranded, often blunt-ended, DNA breaks [11]. Beta-radiation results in fewer than 20 ion pairs per micrometer and the traversal of a single beta-particle causes only single stranded DNA breaks, whereas higher absorbed doses are needed to achieve double-stranded breaks, and then often with cohesive ends [11]. Because alpha particles have a short range (approximately 0.05-0.1 mm in human tissue vs several millimeters (0.05-12mm) for beta particles [7,10]), α-particles deliver a large amount of radiation to target tissue while relatively sparing normal surrounding tissue [5]. With beta particles, neighboring cells around the targeted cell are also irradiated (cross-fire effect) which is considered advantageous for targeting large tumors with a heterogeneous target distribution, but can have a negative effect on adjacent normal cells (such as bone marrow cells) [10]. As a result of the short range of α emissions, there should be less hemotoxicity from α emitters compared to beta emitters [1]. The high linear energy transfer of the α particle, compared to a beta emission (80-100 keV/µm (50-230 keV/µm [10]) versus 0.2 keV/µm [7,9]), also results in greater biological effectiveness with more irreversible double-stranded DNA breaks per unit absorbed dose that cells cannot repair and hence the damaged cells succumb to apoptosis [1,2,7]. The range of the particles (<100 um or a few cell diameters) is also shorter than the 0.7 cm path of 89Sr and the 0.33 cm path of 153Sm, which results in less irradiation to health tissue [1,2,9]. The cytotoxicity of α-emitters is also independent of cell cycle or oxygen concentration, providing an advantage for treating hypoxic, often radioresistant tumors [14].
With regards to radiation exposure, a patient of average weight receiving 3.5 mBq of 223Ra-dichloride will emit radiation at a rate of 0.35 mSv/hr at one meter immediately following administration which entails minimal radiation safety precautions [7]. There are no contact precautions with the agent, but bathroom precautions are recommended (fecal excretion is the primary mode of clearance [7]) for one week and include multiple flushing and area clean up [5].
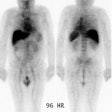
The agent is rapidly cleared from the blood with less than 1% remaining at 24 hours [1,4]. Most if the administered activity is rapidly taken up by bone (61% at 4 hours) [4]. The agent has physiologic similarities to calcium and accumulates in the bone matrix in proportion to the extent of bone metabolism/osteosclerotic bone remodeling [8,16]. Elimination is mainly through the GI tract (fecal elimination) with the median being 52% activity in the bowel at 24 hours [1,4,5]. Other authors suggest that nearly half of the administered activity accumulates within minutes in the GI tract [13]. Despite this, there is low GI tract toxicity [4], but this accumulation reduces activity reaching sites of disease [13]. It has been suggested that the use of amiloride, an epithelial sodium ion channel blocker, can result in decreased gut excretion and improved bioavailability of the agent [13]. Urinary excretion is minimal (typically < 5%) [1]. Limited imaging can be obtained from gamma emissions from 223Ra (1.1% abundance) and its daughter products [1,4].
Administration is based on body weight with a dose of 50 kBq/kg (1.35 uCi/kg) given as repeated injections for 6 doses [1]. For the first dose, the ANC should be 1.5 x 109/L or greater, the platelet count 100 x 109/L or greater, and the hemaglobin at least 10 g/dL or higher [1]. For subsequent doses, the ANC should be 1.0 or higher and the platelet count 50,000 or higher [1]. The agent should be discontinued if hematologic values do not recover within 6-8 weeks after the last administration despite supportive care [1].
Results:
The agent is presently approved for use in patients with bone metastases from castration resistant prostate cancer (and no known visceral metastatic disease) [1]. The existence of any visceral metastases is a contraindication and bone marrow involvement should also be a contraindication [6]. 223Ra therapy is effective in providing pain relief which can be seen in 52% of patients at 1 week, 60% at 4 weeks, and 56% at 8 weeks [1]. The greatest benefit in pain reduction is associated with patients that receive 5-6 injections [17]. Bone alkaline phosphatase (ALP) is a marker for tumor response in these patients and a significant decrease in ALP is seen following 223Ra therapy (a decrease in ALP is more common than a decline in PSA [5]) [1]. A significant decrease in PSA levels also occurs following therapy (compare to placebo) [1]. However, lack of a PSA decrease does not indicate therapeutic failure and therapy should not be stopped prematurely [5,6]. The decision to discontinue treatment should be based on clinical symptomatology, therapeutic tolerability, and radiographic evidence of progression [6]. An approximately 3.6 month survival benefit has also been demonstrated in one study (14 vs 11.2 months) [1,5].
Although 223Ra therapy has been shown to improve survival, there is heterogeneity of response, with some patients showing a limited or poor response [3]. Some lesions on bone scan can improve following treatment [8]. 223Ra kills with maximum efficiency prostate cancer cells proximal to the bone surface (within 100 um), whereas it leaves the distant core unperturbed [15]. On the basis of this zonal toxicity, 223Ra therapy is most effective when applied to lesions of limited size [15]. Some have proposed the combination of 223Ra with other agents that radiosensitize prostate cancer cells to enhance its efficacy [15].
The initial skeletal tumor burden identified on bone scan or 18F-flouride PET/CT has been correlated with worse overall survival following 223Ra therapy [3,8,12]. Additionally, high tumor involvement of bone identified on bone scan has also been shown to be associated with a greater likelihood of inability to complete 223Ra treatment due to disease progression or cytopenia [12]. Patients with lower TTVbone on pre-therapy Ga-68 PSMA PET imaging have been shown to have better clinical outcomes after 223Ra treatment [18].
In cases of disease progression after the initial 6 cycles of 223Ra therapy, a re-challenge with a second course of six 223Ra seems to be feasible, with minimal hematologic toxicity and sustained benefit in terms of overall survival [16].
Other factors associated with worse survival include an ALP greater than 146 U/L, a pain score greater than 3, skeletal related events, a PSA greater than 10 ng/mL, a hemoglobin less than 12.8 g/dL, visceral or nodal metastases, and older age [3].
Complications/Side effects:
The most common adverse reactions (>10%) are nausea, vomiting, diarrhea, and peripheral edema [5], as well as fatigue and bone pain, some of which are dose-related [16].
Hematopoietic toxicity is dose-related with a nadir occurring 2-4 weeks after treatment [1]. Grade 3 and 4 thrombocytopenia has been reported in 6% of patients [16]. Generally, recovery occurs by 24 weeks [1]. It has been suggested that a greater extent of skeletal metastatic disease on bone scan is a significant risk factor for developing hematologic toxicity [8].
Combination use of 223Ra with abiraterone and prednisone (or prednisolone) has been associated with an increased risk for fractures [12].
Long-term followup for the agent is not yet available, but to date no myelodysplastic syndrome, aplastic anemias, or leukemias have been observed [1]. In one study, only 25% of patients were able to complete the entire 6-dose treatment regimen [5]. Advancing soft tissue disease is one of the primary reasons for cessation of therapy [5].
There is an increased risk for fractures (29% vs 11%) and a trend toward increased mortality (30.7 months vs 33.3 months) in patients who receive 223Ra in combination with abiraterone and prednisone [16]. There is limited data regarding the time interval between therapy with abiraterone and 223Ra, but it is recommended that 223Ra be started no earlier than 5 days after the last administration of abiraterone [16]. Subsequent systemic cancer therapy should be initiated no earlier than 30 days after the last dose of 223Ra [16]. Concurrent use of bisphosphonates or denosumab has been found to reduce the incidence of fractures in patients treated with 223Ra [16].
Therefore- 223Ra should be used only in patients as a monotherapy or in combination with a luteinizing hormone-releasing hormone analog in the treatment of symptomatic bone metastases and no known visceral metastases [16]. It is not recommended in patients with low level osteoblastic bone mets or in asymptomatic patients [16].
REFERENCES:
(1) J Nucl Med 2014; Pandit-Taskar N, et al. Bone-seeking radiopharmaceuticals for treatment of osseous metastases, part 1: α therapy with 223Ra-dichloride. 55: 268-274
(2) AJR 2014; Wadas T, et al. Molecular targeted α-particle therapy for oncologic applications. 203: 253-260
(3) J Nucl Med 2015; Etchebehere EC, et al. Prognostic factors in patients treated with 223Ra: the role of skeletal tumor burden on baseline 18F-flouride PET/CT in predicting overall survival. 56: 1177-1184
(4) J Nucl Med 2015; Chittenden S, et al. A phase 1, open-label study of the biodistribution, pharmaokinetics, and dosimetry of 223Ra-dichloride in patients with hormone-refractory prostate cancer and skeletal metastases. 56: 1304-1309
(5) J Nucl Med 2016; Iagaru AH, et al. Bone-targeted imaging and radionuclide therapy in prostate cancer. 57: 19S-24S
(6) J Nucl Med 2017; Ahmadzadehfar H, et al. 68Ga-PSMA-11 PET as a gatekeeper for the treatment of metastatic prostate cancer with 223Ra: proof of concept. 58: 438-444
(7) AJR 2017; Jadvar H. Targeted radionuclide therapy: an evolution toward precision cancer treatment. 209: 277-288
(8) J Nucl Med 2018; Fosbol MO, et al. 223Ra therapy of advanced metastatic castration-resistant prostate cancer: quantitative assessment of skeletal tumor burden for prognostication of clinical outcome and hematologic toxicity. 59: 596-602
(9) J Nucl Med 2018; Poty S, et al. α-emitters for radiotherapy: from basic radiochemistry to clinical studies- part 1. 59: 878-884
(10) J Nucl Med 2019; Nicolas GP, et al. New developments in peptide receptor radionuclide therapy. 60: 167-171
(11) J Nucl Med 2020; Kratochwil C, et al. Patients resistant against PMSA-targeting alpha-radiation therapy often harbors mutations in DNA damage-repair-associated genes. 61: 683-688
(12) J Nucl Med 2021; Dittmann H, et al. The prognostic value of quantitative bone SPECT/CT before 223Ra treatment in metastatic castration-resistant prostate cancer. 62: 48-54
(13) J Nucl Med 2021; Abou DS, et al. Improved 223Ra therapy with combination epithelial sodium channel blockade. 62: 1751-1758
(14) J Nucl Med 2022; Yang H, et al. Harnessing α-emitting radionuclides for therapy: radiolabeling method review. 63: 5-13
(15) J Nucl Med 2022; Paindelli C, et al. Enhancing 223Ra treatment efficacy by anti-ß1 integrin targeting. 63: 1039-1045
(16) J Nucl Med 2023; Feuerecker B, et al. Clinical transformation of targeted α-therapy: an evolution or a revolution? 64: 685-692
(17) J Nucl Med 2023; Palmedo H, et al. Pain outcomes in patients with metastatic castration-resistant prostate cancer treated with 223Ra: PARABO, a prospective noninterventional study. 64: 1392-1398
(18) J Nucl Med 2023; de Jong AC, et al. 68Ga-PSMA PET/CT for response evaluation of 223Ra treatment in metastatic prostate cancer. 64: 1556-1562
PSMA radioligand therapy:
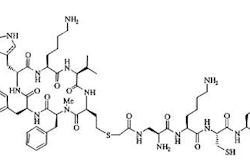
PSMA (also known as hydrolase 1 [FOLH1]) is a type II transmembrane glycoprotein that is over-expressed in metastatic prostate cancer and the degree of PSMA expression positively correlates with tumor stage [1,2,133]. However, the ligand is not specific to the prostate gland and is expressed on other normal tissues including the normal prostate epithelium, salivary and lacrimal glands, duodenal mucosa, proximal renal tubular cells, nonmyelinated ganglia, and neuroendocrine cells in the colon crypts [1,2,133]. It is also expressed on certain neoplasms including transitional cell carcinoma, renal cell carcinoma, and colon cancer [1].
177Lu-PSMA:
177Lu has a short range medium energy beta-particle, a relatively long half-life of 6.7 days, and a low-energy gamma emission that enables RNT administration in an ambulatory setting, as well as post-treatment dosimetry [133]. Radionuclide therapy with agents such as 177Lu-labeled PSMA, although not curative, may be considered in patients who have confirmed progressive castrate resistant prostate cancer after exhaustion of approved therapies, including patients previously treated with taxane agents [2,58,95,105]. 177Lu-PSMA is a low molecular weight ligand that binds to the cell surface of prostate carcinoma cells and is transported into the cell by receptor-mediated endocytosis [114]. The 497-keV beta-energy of 177Lu corresponds to a mean and maximum tissue range of only 0.5 and 2 mm (10-50 cell diameters), respectively [58]. The agent has a long effective half-life in both skeletal and soft tissue metastases, approaching the physical half-life of 177Lu and this results in a high mean absorbed tumor dose (the maximum doses obtained in lymph node mets was 468 Gy and in bone mets 260 Gy) [127]. Other authors quote dose estimates between 1.2-47.5 Gy/GBq (mean 13.1 Gy/GBq) [76]. The red marrow dose is low (0.03 Gy/GBq) [76]. Organs at risk are the kidneys (0.5-0.7 Gy/GBQ) and the salivary or lacrimal glands (1.2-28 Gy/GBq) [76].
Treatment: Prerequisites for treatment include a history of metastatic castrate resistant prostate cancer [130]. Patients should have confirmed PSMA expression by the tumor and metastatic foci- ideally demonstrated by baseline PSMA-directed imaging (such as with 68Ga-PSMA PET/CT) and with lesion uptake greater than or equal to that of liver background activity [2,130,132] as this results an overall survival benefit in the largest cohort of patients [147]. Tumor dedifferentiation leads to loss of PSMA expression, which is typically heterogeneous [143]. In one study, fewer than 10% of patients with low or no PSMA expression at baseline were shown to have a significant response to PSMA therapy [132]. Patents should have absence of lesions that are both PSMA negative and FDG positive and dual tracer screening prior to treatment has been advocated [130,131]. FDG avid disease represents sites of aggressive disease that cannot be efficiently targeted with radioligand therapy [131]. Lesions with low PSMA expression and high glycolytic activity (PSMA negative/FDG positive) can occur in up to 30% of metastatic castrate resistant prostate cancer patients referred for PSMA-targeted therapy [132]. Liver metastases often undergo neuroendocrine trasndifferentiation and are associated with a worse overall survival rate and require dedicated treatment [143].
Radiation dosimetry has shown that the SUVmean on 68Ga-PSMA imaging correlates with absorbed tumor dose [8], a higher lesion SUVmax on imaging correlates with greater likelihood of a PSA response [130], and a higher mean SUV on pretreatment imaging is predictive of longer overall survival [130], and a higher whole-body PSMA SUVmean on baseline PET is associated with better outcomes with 177Lu-PSMA therapy [147].
Patients should have a sufficient bone marrow reserve with a hemoglobin of at least 8g/dL, a white blood cell count more than 2.0 x 109/L, an absolute neutrophile count of at least 1.0 x 109/L, and a platelet count of more than 75,000, good renal and liver function (urinary tract obstruction increases the risk for excessive radiation dose to the kidneys), and no potentially myelosuppressive therapy for more than 6 weeks [2,147]. Patients should have laboratory testing within 2 weeks of planned treatment [2]. Patients should be effectively castrate for the duration of PSMA RLT and ARPIs such as abiraterone or enzalutamide can be safely continued during treatment [147]. In addition, if patients stop or start ARPIs during treatment, the PSMA response may not be reliable, as the androgen receptor controls PSA secretion from tumor cells [147].
The standard regimen consists of IV infusions of 177Lu-PSMA for 4 cycles, with an additional two cycles (5 and 6) administered to patients having evidence of a beneficial response without dose-limiting toxicity [139,147]. Most sites use a standard activity of 6.0 to7.4 GBq and an 8 week interval between treatments [2]. Results appear to be favorable and comparable with either activity regimen with similar PSA response rates [134]. Organs at risk for a critical radiation dose are the lacrimal, parotid, and salivary glands (salivary gland dose is 1.4 Gy/GBq) and kidneys (0.75 Gy/GBq) [1,2]. Ice packs for the salivary glands may be considered to reduce blood flow [2]. PSMA inhibitors such as 2-(phosphonomethyl) pentanedioic acid have been proposed to diminish renal PMSA binding [1]. In the future, treatment my be individually optimized for each patient by considering factors such as tumor burden, dosimetry, and pretreatments [144].
On ligand binding, PSMA and its bound molecule are internalized via clathrin-coated pits and subsequent endocytosis [3]. While the beta-emitting component of 177Lu is utilized for therapy, the gamma component can be used for imaging [3]. A drawback of the agent is that 50% of the administered activity is excreted within 4 hours of administration and nearly 70% by 12 hours [7].
Results:
Studies have shown that there is significantly higher absorbed doses in lymph node and osseous lesions in responders compared to non-responders [151]. After the first treatment cycle for lymph node metastases the mean absorbed dose in responders was 3.73+/- 1.65 Gy/GBq vs 1.86+/-1.25 Gy/GBq in non-responders, and for bone metastases 3.47+/-2.00 Gy/GBq and 1.48+/-0.95 Gy/GBq [151]. The highest absorbed dose was observed after the first treatment cycle, and decreased on subsequent therapies [151]. Patients with higher lesion uptake on baseline imaging (two or more times higher than renal activity) demonstrated a higher response rate [151].
A comparative meta-analysis has suggested that 177Lu-PSMA therapy is less toxic, induces higher PSA response rate, and possibly improves overall survival (14 months vs 12 months) compared to other third-line treatments for mCRPC, such as enzalutamide and cabazitaxel [134].
Between 59-80% of patients will demonstrate some decline in PSA levels following therapy [85,95,108,109,127].
A decrease in PSA of 50% or more (considered a biochemical response) can be seen in 32-64% of patients and this decline can be seen as early as after the first cycle of treatment [1,2,8,85,95,108,109,127]. Early changes in PSA following therapy have also been shown to be indicators of long term clinical outcome [128,133] with a decline in PSA after the first cycle of treatment associated with prolonged survival [2]. In a phase 2 trial, OS was longer in patients who experiences a PSA decline of 50% or greater [134]. In another study following 177Lu-PSMA therapy, a greater than or equal to 30% decline in PSA values at 6 weeks after treatment was associated with a longer survival (16.7 months) compared to patients with stable PSA (11.8 months) or PSA progression (6.5 months) [128]. PSA flare appears to be very uncommon after 177Lu-PSMA treatment, as opposed to therapy with taxanes which can be associated with a PSA flare in 20% or more of patients (a PSA flare is defined as a PSA increase of 25% in the first 6 weeks after therapy followed by a decline below baseline levels at 12 weeks) [128].
In one study following treatment, the median progression-free survival was 13.7 months and the median overall survival was not reached during a 28 month followup period [127]. In another study, patients that achieved a PSA decline of at least 50% had a median survival of 18.4 months (compared to 8.7 months if the PSA decline was less than 50%) [8]. In the VISION trial. there was longer median radiographic progession free survival (8.7 vs 3.4 mo) and longer overall survival (15.3 vs 11.3 mo) for 177Lu-PSMA-617 therapy versus the standard of care, respective, in PSMA-positive mCRPC after the use of taxane and next generation androgen receptor signaling inhibitor agents [137]. A meta-analysis has suggested an improved median survival in 177Lu-PSMA treated patients of 2.5 months [109].
In a study of patients with castration resistant prostate cancer treated with 177Lu-PSMA and a radiation sensitizer (NOX66) 70% of patients had a PSA response of more than 50% [140]. Findings associated with a worse prognosis on post-treatment imaging included an increase in PSMA TTV of at least 30% (on PSMA imaging) and increasing SUVmax on FDG imaging [140]. In this study, reduced PSMA SUVmax occurred in almost all patients in response to 177Lu-PSMA therapy and was not predictive of either treatment response or OS [140]. This may be because 177Lu-PSMA preferentially targets highly PSMA-expressing cells, leading to persistent populations of low-PSMA expressing disease that may be less responsive to treatment [140]. However, patients that were shown to have an increase in PSMA TTV at trial exit, had a PSMA SUVmax of more than 15, significantly higher than in patients without progressive disease, and above a range at which PSMA-targeted therapy is expected to be effective [140]. Accurate assessment of change in PSMA TTV can be difficult, especially in patients with high volume disease [140].
Patients with PSMA negative lesions on screening PSMA PET (VISION screening failure patients) that undergo 177Lu-PSMA therapy have been shown to have a lower rate of over 50% decline in PSMA and shorter overall survival (9.6 months vs 14.2 months) [138]. In another study the survival was 7.5 months compared to 12.4 months [143]. Lesions with low or absent or low PSMA expression likely limits the response to PSMA directed therapy and have been shown to be associated with short overall survival time [138,143]. However, the best management of patients with both PSMA positive and negative lesions is unknown- these patients may benefit from the synergistic effects of combination therapy with stereotactic XRT to the non-PSMA lesions together with PSMA-targeted therapy [138].
There is a significant correlation between whole-body tumor dose (estimated by pre-treatment 68GA-PSMA imaging) and PSA response [5]. One study noted that a mean whole-body tumor dose of 14.7 Gy was associated with a PSA response of at least 50% at 12 weeks [133]. Patients that receive less than a 10 Gy tumor dose are unlikely to achieve a fall in PSA of at least 50% [5]. Post treatment dual time point SPECT/CT imaging may be used to evaluate for 177Lu-PSMA tumor retention [148]. One study suggested that patients with a greater decreased percentage of the injected dose between scans was associated with non-response to treatment, shorter progression free survival, and shorter overall survival [148]. Kinetics analysis suggests a more significant drop in activity could be linked with faster tracer washout from the cells and therefore a shorter radiopharmaceutical residence time, which results in a smaller delivered dose [148].
Due to a tumor sink effect, patients with larger tumor burdens appear to have lower salivary and renal absorbed doses, which may permit higher administered activities for therapy [5].
Following treatment, in one study, 56% of patients with measurable soft-tissue disease achieved an objective response by RECIST 1.1 [8]. However, PSMA PET imaging may be a better predictor of response [131].
Post-treatment whole body SPECT/CT at 24 hours after therapy can also be performed and the results can carry prognostic significance [141]. Patients with high scintigraphic tumor uptake show a higher PSA response rate of at least 50% (45.7% vs 10.4%) and a reduced risk of PSA progression [141]. Overall survival is also significantly longer in patients with high tumor uptake in the absence of visceral metastases (15.5 months vs 11.4 months) [141]. Patients that demonstrate a scinitgraphic response (defined as a decrease in skeletal infiltration length between two cycles) have a significantly higher likelihood for a PSA response (64%) and a significantly longer PSA PFS (33 weeks), and a longer median OS (16.5 months) [141]. Any increase in SPECT TTV between baseline and week 6 is associated with a significantly shorter PSA PFS [142]. Note that an increase in SPECT TTV at week 6 can be seen even in patients without a rise in PSA level (up to 25% of patients can show progressive TTV and no increase in PSA) [142]. The combination of increase SPECT TTV and a PSA rise at week 6 identifies a subgroup of patients with a high risk of poor response to 177Lu-PSMA therapy and may benefit from a change in therapy or addition of combination therapy [142].
Pain relief can be seen in 33-70% of patients, an improved quality of life in 60%, and improved performance status in 74% [2]. Another study also demonstrated significant improvement in quality of life during the course of treatment with 177Lu-PSMA [152].
However, one third (20-40%) of patients do not respond despite the presence of PSMA over-expression on pre-therapy PET scans [3,76] and therefore, SUVmax on 68Ga-PMSA imaging is not a predictor of response to therapy [95]. Certain biomarkers are associated with resistance to 177Lu-PSMA therapy [149]. In particular, amplifications in CCNE1 (31% vs 0%) and FGFR1 (25% vs 0%), and CDK12 mutations (25% vs 4 %) were more likely to be present in non-responders [149]. CCNE1 over-expression is associated with worse overall survival, progression free survival, and distant metastatic disease free survival in multiple malignancies [149]. CCNE1 upregulation is also associated with platinum-based therapy resistance in ovarian, endometrial, and bladder cancers [149]. The FGFR1 amplification is associated with up-regulation of fibroblast growth factor receptor 1, which is responsible for the activation of multiple downstream oncogenic pathways and correlates with resistance to certain cyclin-kinase inhibitors in breast cancer [149]. CDK12 mutations are known to have adverse effects on prognosis in patients with mCRPC [149].
Factors associated with a better likelihood for a biochemical response include an alkaline phosphatase level of less than 220 U/L and the absence of visceral metastases [95]. Better overall survival following treatment is seen in patients that demonstrate a PSA decline in 2 months following the first cycle of therapy [95]. Interestingly, about 88-93% of patients with a PSA response after the first cycle will respond to further cycles, but up to 40% of non-responders may also respond to further therapy cycles [95].
The presence of any visceral metastases or a serum alkaline phosphatase 220 U/L or higher (an indication of more advanced bone marrow involvement) are predictive of a poor outcome [2].
In one study of patients with mCRPC undergoing 177Lu-PSMA therapy, at least one mismatch PSMA-negative/FDG-positive metastases was noted in 59% of patients and this mismatch was associated with a significant shorter overall survival compared to patients without mismatch lesions [136]. Mismatched lesions are associated with a Gleason score of 8 and a serum PSA level of 7.9 ng/mL [136]. Serum neuron-specific enolase concentration (a cytoplasmic marker for tumors of neuroendocrine origin) has been shown to be significantly and positively associated with FDG-avid and low PSMA-expressing metastases in patients with mCRPC [136].
The total number of docetaxel cycles has been shown to be an independent factor for overall survival- patients who received more than 10 cycles have been shown to have a higher median survival [139].
In chemotherapy naive mCRPC patients:
One study of patients with mCRPC without prior chemotherapy randomized patients to treatment with docetavel versus 177Lu-PSMA [150]. The mean OS for each group was 15 months- indicating that early initiation of 177Lu-PSMA treatment is not inferior to chemotherapy [150]. Previous studies have also demonstrated a similar biochemical response and there are fewer grade 3 or higher adverse events associated with 177Lu-PSMA therapy [150]. Another meta-analysis comparing the efficacy outcomes in chemotherapy-naive versus chemotherapy treated patients, taxane-naive patients had a 1.8 times improved odds of a biochemical recurrence, a 40% reduced risk of progression, and a 46% reduced risk of death after radioligand therapy compared to taxane-treated patients [150].
When to discontinue treatment:
In general, it is important to administer 2 cycles before assessing response [147]. While there are not clearly defined rules regarding treatment failure, three factors should be considered- imaging-based progression, PSA progression, and clinical decline [147]. These three factors are not always in sync and patients can have imaging progression while clinically improving [147]. A rising PSA with worsening clinical symptoms or imaging progression may indicate that therapy should be discontinued [147]. The development of new liver lesions on therapy should be an indication to stop treatment [147].
Effect of prior therapy:
The TheraP trial demonstrated better biochemical and radiologic response outcomes, as well as longer PFS, with 177Lu-PSMA therapy than with cabazitaxel in mCRPC patients that previously progressed on doxetaxel [145].
In a metaanalysis of patients with metastatic castration resistant prostate cancer receiving 177Lu-PSMA treatment, patients with no prior taxane treatment had significantly better outcomes compared to previously taxane treated patients [145]. The PSMA response rate was 57% of taxane-naive patients versus 40% for patients that had received prior taxane therapy [145]. Lack of prior taxane therapy was also associated with better progression free survival [145]. Specifically- in taxane-naive patients receiving 177Lu-PSMA therapy, the odds of having a PSA response were 1.8 times better than for taxane-treated patients, with a reduction of 40% and 46% in the risk of progression and death, respectively [145].
Relapse:
177Lu-PSMA re-treatment in initial responders who ultimately relapse has been performed [6,8]. In one study, a PSA decline of at least 50% was seen in 73% of retreated patients, but the duration of response was shorter (no increased adverse effects were observed) [8]. Another study suggested that re-treatment has a lower efficacy and higher toxicity [6]. In that study, only 38% of patients demonstrated a 50% PSA decline and the median progression free survival was 3.3 months, compared to 12.4 months following the initial course of therapy [6].
Progressive disease following treatment most commonly involves the marrow (56% of cases) or liver (19% of cases) [8]. Progressive liver disease in these patients generally demonstrates low PSMA expression and high metabolic activity [8].
New discordant PSMA-negative/FDG-positive lesions can develop following 177Lu-PSMA therapy in up to 13% of patients [136].
Combination therapy:
Despite anti-tumor activity associated with PSMA radionuclide therapy (RNT), all patients invariably develop recurrence [133]. Combination radionuclide therapy augmented with other treatment modalities can have a synergistic effect [133].
Androgen receptor (AR) blockade may synergize with PSMA-RNT [133]. First- AR blockade has been reported to sensitize to radiotherapy by delaying DNA repair through temporal prolongation of repair factory complexes and halting the cell cycle [133]. Second, AR blockade has been shown to modulate the expression of PSMA, although the exact effect of AR blockage on PSMA expression hinges on the state of castration [133]. AR blockage has dichotomous effects - in patients with hormone-sensitive prostate cancer, a significant reduction in 68Ga-PSMA intensity occurred in 86% of men as early as 9 days after starting androgen blockage [133]. Whereas in patients with CRPC, AR blockade caused in increase in PSMA expression [133]. Third, treatment with enzalutamide, dutasteride, and rapamycin has been shown to increase the uptake and internalization of 177Lu-PSMA in prostate cancer cell lines [133].
RNT may be combined with chemotherapy- taxane agents can radiosensitize tumors [133]. Another combination treatment may involve RNT, which produces cell damage through DNA strand breaks, with agents that inhibit DNA repair [133].
Side effects/Complications:
One of the major disadvantages of PSMA-radioligand therapy is the high accumulation of the agent in non-target tissues [129]. The PSMA receptor is also expressed in high levels on certain normal tissues including the proximal tubules of the kidneys, the brush border of the jejunum, and the salivary and lacrimal glands [114].
Xerostomia (Dry mouth)- Grade 1 dry mouth has been reported in up to 87% of patients [108] and grade 1-2 in 66% of patients [8], typically self-limiting. The risk for dry mouth is slightly greater for the 7.4 GBq treatment dose compared to the 6.0 GBq dose (63% vs 58%) [135]. External cooling does not appear to reduce tracer uptake by the parotid glands [114].
Orally administered monosodium glutamate (MSG) has been shown to significantly decrease salivary gland, kidney, and other normal-organ uptake, but it also produces a decrease in tumor uptake as well [129].
Nausea- Grade 1-2 transient nausea can be seen in 50% of patients [8,108]. Typically within the first 24 hours of therapy, transient, and manageable with antiemetics [8].
Diarrhea- has been reported in 13% of patients treated with 6.0 Gbq and 32% of patients treated with 7.4 GBq [135].
Anemia/Leukopenia/Thrombocytopenia- Serious hematologic adverse events can be seen in up to 12% of patients [2]. A low blood cell count at baseline and diffuse bone marrow involvement pose a risk for serious hematotoxicity [2]. Grade 3 or 4 anemia (3-10%), neutropenia (1-10%), leukopenia in 3%, lymphopenia (32%), and/or thrombocytopenia (2-13%) of patients, respectively [1, 8,105,108,135].
A complete blood count and metabolic panel should be checked at least every 6 weeks and more frequently in patients with lower bone marrow counts [147]. The PSA level should be checked at least every 6 weeks [147].
Renal toxicity- The primary route of 177Lu-PSMA excretion is renal [153]. Cumulative absorbed renal does between 15 Gy and 31 Gy have been reported depending on the number of cycles of treatment the patient receives [153,154]. Grade 1-2 renal injury can be seen in 4.5-12% of patients [8,135]. Grade 3 of higher renal toxicity is a very rare complication seen in about 3.4% of patients (note that in the VISION trial grade 3-5 real dysfunction was observed in a comparison group of patients receiving standard of care therapy alone) [105,154]. However, other authors report higher levels of renal dysfunction, particularly in patients with longer term follow-up [154]. In that study, 45% of patients who received 4 or more cycles of therapy, demonstrated a decrease in eGFR of at least 15% from baseline at 12 months following treatment, and more than half of those had a decrease of 30% or more (representing 24% of the patient cohort) [154]. In patients with no or only mild decrease in eGFR (<15%) at 12 months, had a more than 15% decrease in GFR by 24 months [154]. Other authors point out that a direct causality between 177Lu-PSMA therapy and renal dysfunction is difficult to confirm due to multiple prior lines of therapy, co-morbidities, and underlying advanced metastatic malignancy that can also contribute to renal dysfunction in these patients [155].
Underlying chronic kidney disease, diabetes, age >/= 65 years, and hypertension are increased risk factors for renal toxicity [135,154]. The more risk factors that are present, the greater the risk of renal dysfunction [154].
Mannitol infusion is a strategy to reduce renal uptake by acting as an osmotic diuretic, decreasing renal reabsorption [129].
Pain flare
Hypocalcemia: Hypocalcemia may occur in response to 177Lu-PSMA therapy [146]. Risk factors appear to be patients with high volume bone metastases and a significant PSA response (>90% reduction in PSA) [146]. This may be related to an uncoupling of bone turnover favoring bone formation with an increased skeletal demand for calcium that depletes circulating calcium stores [146].
It should be noted that chemotherapy with docetaxel can also result in toxic side effects in up to 67% of patients, including grade 3-4 myelosuppression in 32-47% of patients [135] and cabazitaxel chemotherapy can result in grade 3 or greater neutropenia in 45% of patients [135]. Other toxicities include GI toxicity (0-60%), cardiac toxicity (24-48%), and treatment related death (0.3%) [109].
REFERENCES:
(1) AJR 2017; Jadvar H. Targeted radionuclide therapy: an evolution toward precision cancer treatment. 209: 277-288
(2) J Nucl Med 2017; Fendler WP, et al. 177Lu-PSMA radioligand therapy for prostate cancer. 58: 1196-1200
(3) J Nucl Med 2017; Hadaschik BA, Boegemann M. Why targeting of PSMA is a valuable addition to the management of castration-resistant prostate cancer: the urologist's point of view. 58: 1207-1209
(4) J Nucl Med 2018; Rathke H, et al. Repeated 177Lu-labeled PSMA-617 radioligand therapy using treatment activities of up to 9.3 GBq. 59: 459-465
(5) J Nucl Med 2019; Violet J, et al. Dosimetry of 177Lu-PSMA-617 in metastatic castration-resistant prostate cancer: correlations between pretherapeutic imaging and whole-body tumor dosimetry with treatment options. 60: 517-523
(6) J Nucl Med 2019; Gafita A, et al. Early experience of rechallenge 177Lu-PSMA radioligand therapy after intial good response in patients with advanced prostate cancer. 60: 644-648
(7) J Nucl Med 2019; Kelly JM, et al. Albumin-binding PSMA ligands: implications for expanding the therapeutic window. 60: 656-663
(8) J Nucl Med 2020; Violet J, et al. Long-term follow-up and outcomes of retreatment in an expanded 50-patient single-center phase II prospective trial of 177Lu-PSMA-617 theranostics in metastatic castration-resistant prostate cancer. 61: 857-865 (58) J Nucl Med 2016; Kratochwil C, et al. PSMA-targeted radionuclide therapy of metastatic castration-resistant prostate cancer with 177Lu-labeled PMSA-617. 57: 1170-1176 (76) J Nucl Med 2017; Eiber M, et al. Prostate-specific membrane antigen ligands for imaging and therapy. 58: 67S-76S (85) J Nucl Med 2018; Donin NM, Reiter RE. Why targeting PSMA is a game changer in the management of prostate cancer. 59: 177-182 (95) J Nucl Med 2018; Ahmadzadehfar H, Essler M. Predictive factors of response and overall survival in patients with castration-resistant metastatic prostate cancer undergoing 177Lu-PSMA therapy. 59: 1033-1034 (105) J Nucl Med 2019; Barber TW, et al. Clinical outcomes of 177Lu-PSMA radioligand therapy in earlier and later phases of metastatic castration-resistant prostate cancer grouped by previous taxane chemotherapy. 60: 955-962 (108) AJR 2019; Subramaniam RM. Prostate cancer theranosis in clinical practice and in clinical trials- 68Ga-prostate-specific member antigen (PSMA)-11 PET/CT and 177Lu-PMSA-617 therapy. 213: 241-42 (109) AJR 2019; Yadav MP, et al. Radioligand therapy with 177Lu-PSMA for metastatic castration-resistant prostate cancer: a systematic review and meta-analysis. 213: 275-285
(114) J Nucl Med 2019; Yilmaz B, et al. Effect of external cooling on 177Lu-PSMA uptake by the parotid glands. 60: 1388-1393
(127) J Nucl Med 2016; Baum RP, et al. 177Lu-labeled prostate-specific membrane antigen radioligand therapy of metastatic castration-resistant prostate cancer: safety and efficacy. 1006-1013
(128) J Nucl Med 2020; Gafita A, et al. Early prostate-specific antigen changes and clinical outcome after 177Lu-PSMA radionuclide treatment in patients with metastatic castration-resistant prostate cancer. 61: 1476-1483
(129) J Nucl Med 2021; Harsini S, et al. The effects of monosodium glutamate on PSMA radiotracer uptake in men with recurrent prostate cancer: a prospective, randomized, doble-blind, placebo-controlled intraindividual imaging study. 62: 81-87
(130) Radiology 2021; Lawhn-Heath C, et al. Prostate-specific membrane antigen PET in prostate cancer. 299: 248-260
(131) J Nucl Med 2021; Farolfi A, et al. Current and emerging clinical applications of PSMA PET diagnostic imaging for prostate cancer. 62: 596-604
(132) J Nucl Med 2021; Calais J and Czernin J. PSMA expression assessed by PET imaging is a required biomarker for selecting patients for any PSMA-targeted therapy. 62: 1489-1491
(133) J Nucl Med 2021; Sandhu S, et al. Radionuclide therapy in prostate cancer: from standalone to combination PSMA theranostics. 62: 1660-1668
(134) J Nucl Med 2021; Calais J, et al. Prospective phase 2 trial of PSMA-tageted molecular radiotherapy with 177Lu-PSMA-617 for metastatic castration-resistant prostate cancer (RESIST-PC): efficacy results of the UCLA cohort. 62: 1440-1446
(135) J Nucl Med 2021; Calais J, et al. Safety of PSMA-targeted molecular radioligand therapy with 177Lu-PSMA-617: results from the prospective multicenter phase 2 trial RESIST-PC (NCT03042312). 62: 1447-1456
(136) J Nucl Med 2022; Jadvar H, et al. The VISION forward: recognition and implication of PSMA-/18F-FDG + mCRPC. 63: 812-815
(137) J Nucl Med 2022; Feuerecker B, et al. Pretherapeutic comparative dosimetry of 177Lu-rhPSMA-7.3 and 177Lu-PSMA I & T in patients with metastatic castration resistant prostate cancer. 63: 833-839
(138) J Nucl Med 2022; Hotta M, et al. Outcome of patients with PSMA PET/CT screen failure by VISION criteria and treated with 177Lu-PSMA therapy: a multicenter retrospective analysis. 63: 1484-1488
(139) J Nucl Med 2023; Derkin T, et al. 177Lu-PSMA for extended treatment of metastatic castration-resistant prostate cancer. 64: 54-58
(140) J Nucl Med 2023; Pathmanandavel S, et al. The prognostic value of posttreatment 68Ga-PSMA-11 PET/CT and 18F-FDG PET/CT in metastatic castration-resistant prostate cancer treated with 177Lu-PSMA-617 and NOX66 in a phase I/II trial (LuPin). 64: 60-74
(141) J Nucl Med 2023; Karimzadeh A, et al. 177Lu-PSMA-I&T for treatment of metastatic castration-resistant prostate cancer: prognostic value of scinitgraphic and clinical biomarkers. 64: 402-409
(142) J Nucl Med 2023; Nikeith J, et al. 177Lu-PSMA-I&T SPECT quantitation at 6 weeks (dose 2) predicts short progression-free survival for patients undergoing 177Lu-PSMA-I&T therapy. 64: 410-415
(143) J Nucl Med 2023; Seifert R, et al. Is 18F-FDG PET needed to assess 177Lu-PSMA therapy eligibility? A VISION-like single-center analysis. 64: 731-737
(144) J Nucl Med 2023; Brosch-Lenz J, et al. Toward single-time-point image-based dosimetry of 177Lu-PSMA-617 therapy. 64: 767-774
(145) J Nucl Med 2023; Satapathy S,e t al. [ 177Lu] Lu-PSMA-radioligand therapy efficacy outcomes in taxane-naive versus taxane-treated patients with metastatic castration-resistant prostate cancer: a systematic review and metaanalysis. 64: 1266-1271
(146) J Nucl Med 2023; Kumar S, et al. The Tyr phenomenon: a hypocalcemic response in high-volume treatment responders to 177Lu-prostate-specific membrane antigen therapy. 64: 1412-1416
(147) J Nucl Med 2023; Hope TA, et al. SNMMI consensus statement on patient selection and appropriate use of 177Lu-PSMA-617 radionuclide therapy. 64: 1417-1423
(148) J Nucl Med 2023; Straub M, et al. Dual-time-point posttherapy 177Lu-PSMA-617 SPECT/CT describes the uptake kinetics of mCRPC lesions and prognosticates patients outcome. 64: 1431-1438
(149) J Nucl Med 2023; Sartor O, et al. Prediction of resistance to 177Lu-PSMA therapy by assessment of baseline circulating tumor DNA biomarkers. 64: 1721-1725
(150) J Nucl Med 2023; Satapathy S, et al. [ 177Lu] Lu-PSMA-617 versus docetaxel in chemotherapy-naive metastatic castration-resistant prostate cancer: final survival analysis of a phase 2 randomized, controlled trial. 64: 1726-1729
(151) J Nucl Med 2023; Hohberg M, et al. Prediction of response to 177Lu-PSMA therapy based on tumor-to-kidney ratio on pretherapeutic PSMA PET/CT and posttherapeutic tumor-dose evaluation in mCRPC. 64: 1758-1764
(152) J Nucl Med 2023; Karimzadeh A, et al. Improved quality of life in metastatic castration-resistant prostate cancer patients receiving consecutive cycles of 177Lu-PSMA I&T. 64: 1765-1711
(153) J Nucl Med 2024; Herrmann K, et al. Renal and multiorgan safety of 177Lu-PSMA-617in patients with metastatic castration-resistant prostate cancer in the VISION dosimetry study. 64: 71-78
(154) J Nucl Med 2024; Steinhelfer L, et al. Long-term nephrotoxicity of 177Lu-PSMA radioligand therapy. 64: 79-84
(155) J Nucl Med 2024; Kumar ASR, Hofman MS. Unraveling the impact of 177Lu-PSMA radioligand therapy on renal impairment: distinguishing causation from correlation. 64: 85-86
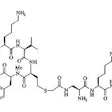
25Ac-PSMA therapy:
Another agent, the alpha emitter 225Ac-PMSA has also been studied for therapy. 225Ac is an alpha emitter with a half life of 9.9 days [1]. Alpha radiation reaches a shorter range (40-100 um) than beta-particles (50-12,000 um), but alpha emitters have a 20-fold higher linear energy transfer compared to beta emitters (up to 0.1-2.2 MeV for alpha particles) [3,6]. The reported linear energy transfer for 177Lu is 0.7 keV/um, compared to 100 keV/um for 225Ac [5]. The result is a more effective radiobiological effectiveness and tumor kill compared to beta-radiation that is largely independent of cell cycle or oxygenation and potentially has less off-target toxicity [5,6].
However, the agent will also have greater on-target damage to healthy tissue including irreversible damage to the lacrimal and salivary glands [6]. 225Ac has six daughter products (221Fr, 217At, 213Bi, 213Po, 209Pb, and 209Tl) with several alpha- and beta decays [1].
Dosing:
Treatment is given at 8 weeks intervals using a dose of 100kBq/kg [7].
PSMA decline:
The agent has been shown to result in a PSA decline of more than 50% in 61-70% (up to 91% of patients [5]) of patients [1,4,8]. The median duration of tumor control is 9 months [1,4]. A PSA decline of 50% or greater has been shown to be significantly associated with overall survival (PFS of 15.2 months and OS of 18-20 months) [1]. Another pilot study demonstrated a greater than 90% decline in PSA in 82% of patients and complete imaging response in 65% of patients [3]. For comparison a 50% or more reduction in PSA is seen in only about 10% of patients treated with ipilimumab, sunitinib, cabozantinib, or 223Ra-dichloride (Xofigo), about 30% of patients treated with abiraterone, 40% treated with cabazitaxel, and 50% treated with enzalutamide [5]. A PSMA decline following 225Ac-PMSA treatment is less commonly seen in patients with late-stage mCRPC [7].
225Ac-PMSA has been used in patients that have become resistant to 177Lu-PSMA therapy [8]. In these patients, a decrease in PSMA levels after one cycle of 225Ac-PMSA was seen in 58% of patients, and 26% of patients demonstrated a decrease in PSMA of over 50% [8]. Median PFS was 3.1 months and overall survival was 7.7 months [8].
Post-treatment imaging findings:
In one study, 68Ga-PSMA exam findings became negative following treatment in 53% of patients [5].
Prognosis:
In a meta-analysis, the estimated mean progression-free survival was 9.15 months and the mean overall survival was 11.8 months [4]. The degree of PSMA decline is predictive of progression and overall survival following therapy [5]. In one study, the median estimated overall survival was 9 months for patients with a PSA decline of less than 50%, but was not reached at 55 months for patients with a decline of 50% or more [5]. The estimated progression free survival was 22 months for patients with a PSA decline of 50% or more, and only 4 months for those with a PSA decline of less than 50% [5]. Patients with higher TTV, late-stage mCRPC and/or liver metastases have a shorter progression free and shorter OS [5,8].
Patients with high baseline immunohistochemical PSMA expression or DNA repair alterations tend to have a longer OS [7]. Interestingly, in one study, a high platelet count was associated with a negative effect on progression free survival [5]. Platelets may interact with tumor cells and endothelial cells enabling metastases [5]. Platelets have been shown to play a role in shielding tumor cells from immune elimination and in protecting cancer cells from undergoing apoptosis [5]. A high pretreatment platelet count has also been associated with a poor prognosis in patients with ovarian, breast, lung, renal, colorectal, and pancreatic cancers [5].
Tandem therapy: Up to 30% of mCRPC patients do not respond to 177Lu-PMSA therapy [7]. In patients resistant to beta-emitters, alpha-emitter therapy may still be effective [7].
Side effects:
Xerostomia: The agent is associated with a high incidence of intolerable xerostomia due to salivary tracer uptake [2]. In a meta-analysis, xerostomia occurred in 63% of patients [4]. Other authors indicate xerostomia in 81-85% of patients (typically grade I or II), but not severe enough to discontinue treatment [1,5]. However, another author indicates that between 10-23% of patients stop treatment due to intolerable xerostomia or in order to preserve quality of life [7].
Dry eyes can also occur [1,4].
Nephrotoxicity: Decrease renal function- grade III or IV renal failure can occur (especially in patients with baseline renal impairment) [1,4,5].
Hemotoxicity: Compared to 177Lu-PMSA, grade 3/4 hematologic toxicity seems higher for 225Ac-PMSA [7]. Anemia is a common toxicity- in a meta-analysis, grade 3 or 4 anemia was observed in 14% of patients (8-35%) [4,5,7]. Thrombocytopenia can occur in 3-19% of patients and leukocytopenia in 1-27%) [4,7].
REFERENCES:
(1) J Nucl Med 2020; Sathekge M, et al. Predictors of overall and disease-free survival in metastatic castration-resistant prostate cancer patients receiving 225Ac-PMSA-617 radioligand therapy. 61: 62-69
(2) J Nucl Med 2018; Kratochwil C, et al. Targeted alpha-therapy of metastatic castrate resistant prostate cancer with 225Ac-PMSA-617: swimmer-plot analysis suggests efficacy regarding duration of tumor control. 59: 795-802
(3) Radiology 2021; Lawhn-Heath C, et al. Prostate-specific membrane antigen PET in prostate cancer. 299: 248-260
(4) J Nucl Med 2022; Lee DY, Kim Y. Effects of 225Ac-labeled prostate-specific membrane antigen radioligand therapy in metastatic castration-resistant prostate cancer: a meta-analysis. 63: 840-846
(5) J Nucl Med 2022; Sathekge M, et al. mCRPC patients receiving 225Ac-PMSA-617 therapy in the post-androgen deprivation therapy setting: response to treatment and survival analysis. 63: 1496-1502
(6) J Nucl Med 2021; Sandhu S, et al. Radionuclide therapy in prostate cancer: from standalone to combination PSMA theranostics. 62: 1660-1668
(7) J Nucl Med 2023; Feuerecker B, et al. Clinical transformation of targeted α-therapy: an evolution or a revolution? 64: 685-692
(8) J Nucl Med 2023; Alan-Selcuk N, et al. Clinical experience with [225Ac] Ac-PMSA treatment in patients with [177Lu] Lu-PSMA refractory metastatic castration-resistant prostate cancer. 64: 1574-1580