Bone Imaging in Neoplastic Disease
Malignant Bone Tumors:
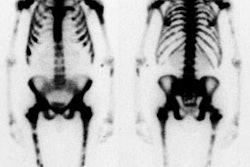
Metastatic Bone Malignancies:
According to the Radiologic Clinics of North America (July 93), bone scan is 50 to 80% more sensitive than radiographs in detecting skeletal metastases. This is probably because about 50% of the bone mineral content must be lost before a met is evident on a radiograph.
For myeloma or very lytic aggressive lesions, however, bone scan is less sensitive. Multiple myeloma lesions are detected about 50% of the time on bone scan, as compared to an 80% detection on skeletal survey. Because of this, skeletal scintigraphy is probably not the procedure of choice for evaluating the presence of skeletal involvement in patients with multiple myeloma or lymphoma.
The specificity of the bone scan in the evaluation of metastatic disease is unfortunately limited as fractures, degenerative disease, or other benign conditions may produce false-positive examinations. Nonetheless, given the ease of performing a whole body survey, bone scan is probably the study of choice for the initial evaluation for mets in patients with cancer.
About 90% of patients with skeletal metastases present with multiple lesions. Nearly 80% of all metastatic lesions are in the axial skeleton. In patients with a known malignancy, 60 to 70% of axial lesions are due to mets, whereas about 40 to 50% of lesions in the extremities or skull are due to mets. A solitary rib lesion has about a 10% probability of representing a met in a patient with a known malignancy [1].
Other authors have concluded that a single lesion has about a 11% probability for being a met in patients with known underlying malignancy (in this study the underlying malignancy was breast cancer). The percentage increased to 35% when 2 new lesions were detected, and reached 100% when 5 new lesions were identified [2]. In multifocal metastatic disease the regional distribution of lesions for common bone seeking primaries (such as breast, lung, and prostate cancer) is: thorax/ribs (37%), spine (26%), limbs (15%), pelvis (15%), and skull (6%).
The 'Flare phenomenon' reflects a favorable response of bone metastases to treatment. Patients are typically asymptomatic and plain films generally show sclerosis of the lesions. The phenomenon is typically seen between 2 weeks to 3 months following therapy, but can rarely be seen as late as 6 months after treatment. In general, it is prudent to wait about 3 months following completion of a new therapeutic intervention prior to repeating the bone scan. The diagnosis of "flare" requires 2 criteria:
- Increased intensity and/or number of lesions on bone scan (Felt to be secondary to increased osteoblastic activity associated with healing)
- Subsequent decrease uptake in these lesions on repeat exam in 2-3 months.
Bone Scan in Breast Cancer:
Bone scintigraphy is more sensitive in detecting metastatic breast carcinoma than plain films, with an average of between 4 to 6 months for conversion of the radiograph after identification of the lesion by bone scan. In breast cancer patients, there is a low positive yield for the bone scan in patients with early stage disease: About 4% (0-18%) for Stage I and 7% (0-32%) for Stage II disease. In patients with Stage III disease, the yield may be as high as 14 to 28%. In patients who have small primary tumors (less than 2 cm), the routine use of preoperative bone scanning in asymptomatic patients is probably unnecessary [3]. Coleman et al (JNM 1988), recommend a baseline bone scan for all patients with Stage II-IV disease. Women with breast cancer who present with bone mets at the time of diagnosis, have a markedly worse prognosis. In patients with breast cancer, 21% of patients relapsed with a solitary bone met, the most common location being the spine. Although bone pain is a common presenting symptom in these patients, up to 30 to 50% of these patients can be asymptomatic. It is important to note that an isolated sternal lesion in a patient with breast cancer has a 75% likelihood of being a met. There is also a strong correlation between the side of the sternal met, the side of the primary breast lesion, and the presence of pathologic internal mammary lymph nodes.
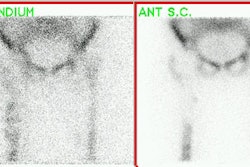
Bone Scan in Prostate Cancer:
In newly diagnosed patients with prostate cancer, patients who have a low PSA (less than 20) have a very low likelihood (less than 1%) of having bone mets. Bone scan should be limited to patients for initial staging with elevated PSA or bone symptoms. Patients who are receiving hormonal therapy (antiandrogen) may have bone mets, even when their PSA is normal.
Primary Bone Malignancies:
The "Extended pattern" refers to increased activity (usually mild to moderate) in adjacent joints or along the entire ipsilateral extremity in association with a primary tumor of a long bone. This finding may be related to generalized increased blood flow to the extremity. It can lead to over-estimation of the extent of the tumor by scintigraphy. Thallium scintigraphy can be used to better define lesion extent and to monitor response to therapy.
Osteosarcoma:
The most common location for primary osteosarcoma is about the knee (50%), followed by the proximal humerus (15%). Common sites for metastases are the lungs and bones. Although pulmonary mets can be detected in 20% (planar imaging) to 40% (SPECT imaging) of patients, skeletal mets are detected in only 3% at the time of presentation. Nonetheless, the presence of skeletal mets is associated with a very poor prognosis and will greatly alter treatment in these patients. A baseline bone scan is generally recommended.
Scinitgraphy is much less sensitive than CT in the detection of pulmonary metastases
(with single headed tomography detecting only 8% of lesions identified by CT in one series
[4]. Although tracer uptake within a pulmonary lesion is very specific for a metastatic
focus of osteosarcoma, the additional cost of tomographic images to detect lung lesions is
difficult to justify, given its lack of sensitivity compared to CT. The use of follow-up
bone scans to detect metastatic lesions is controversial. Some authors feel that skeletal
mets do not occur in the absence of lung metastases and therefore serial bone scans are
not indicated unless new pulmonary lesions are detected on follow-up CT scanning [5].
Others feel bone metastases may be identified before lung mets; possibly due to changes in
the natural course of the malignancy in the face of aggressive chemotherapeutic management
[6]. In this case, and in the detection of other unsuspected remote sites of metastatic
disease, routine followup scintigraphy may be beneficial [7].
Ewing's Sarcoma:
Over 80% of the Ewing's sarcomas occur in patients under 20 years of age, and interestingly blacks are very rarely affected. The tumor usually arises in the diaphysis of a long bone, but 20% arise in the pelvis and lesions in the pelvis are associated with a worse prognosis. The lesion usually produces a "moth-eaten" pattern of bone destruction on plain film radiographs and the lesion is typically "hot" on bone scan. The incidence of skeletal mets at the time of presentation ranges from 10 to 40%. On follow-up, the skeleton is the first site of metastatic disease in about 25% of patients. Baseline, and follow-up bone scans are therefore very useful in these patients.
Benign Bone Tumors:
Aneurysmal Bone Cyst:
Aneurysmal bone cysts (ABC) may also involve the posterior elements of the spine (20-35% of cases). Most of these lesions occur in patients less than 20 years of age. On plain film, an ABC appears as an expansile lytic lesion with a very thin or expanded margin and the lesion may involve more than one contiguous vertebrae. Trabeculations can be seen within the lesion. When the lesion grows rapidly, the reparative process in the bone may lag behind, and the margin of the lesion can appear irregular or interrupted.
On CT or MRI, fluid-fluid levels can be identified in 30% of lesions (although this finding can be seen in other, more aggressive bone lesions as well). On bone scan, increased activity is seen within the lesion on all 3 phases. About two-thirds of the lesions will be photopenic centrally, surrounded by a "ring" of increased activity. Extended uptake is not common.
Bone Island:
About 30% of bone islands will demonstrate increased uptake- particularly large lesions.
Enchondroma:
Enchondromas can have a very variable appearance on bone scan demonstrating very mild,
to rather prominent uptake of tracer. MRI can be used to confirm the presence of a
chondroid matrix within the lesion if plain films are not conclusive.
Osteoblastoma:
Osteoblastomas can also involve the posterior elements of the spine. The lesions are typically larger than 2 cm and possess both sclerotic and lytic features. Plain films typically demonstrate an expansile lytic lesion which contains a calcific matrix. On bone scan, the lesion will be hot on both blood pool and delayed images.
Osteoid Osteoma:
Osteoid osteomas occur most commonly in adolescents and young adults, with 90% of cases seen in patients under age 25. The lesion can be cortical (most common), medullary, or periosteal. The most characteristic clinical presentation is pain, which is worse at night and relieved by aspirin. When the lesion occurs in the spine, it nearly always occurs in the posterior elements (50%) and is frequently associated with a painful scoliosis with the convexity of the curve oriented away from the side of the lesion. The most common location for a spinal lesion is the lumbar spine.
On plain films, the nidus of the lesion (which is highly vascular) is lucent and is surrounded by a zone of dense, reactive sclerosis. MRI demonstrates decreased signal intensity due to the reactive bony sclerosis, but the nidus may produce a brighter signal.
On bone scan, the lesion is hot on all 3-phases. On delayed images the nidus may be seen as a focal area of even greater activity within the diffuse abnormality. Intraoperative localization of the lesion and nidus can be accomplished through the use of a hand held probe. A normal bone scan virtually excludes the diagnosis of an osteoid osteoma.
REFERENCES:
(1) J Nucl Med 1985; Tumeh SS, et al. Clinical significance of solitary rib lesions in patients with extraskeletal malignancy. 26: 1140-1143
(2) J Nucl Med 1990; Jacobson AF, et al. Association between number and sites of new bone scan abnormalities and presence of skeletal metastases in patients with breast cancer. 31: 387-392
(3) Radiol Clin North Am 1993; Brown ML. Bone scintigraphy in benign and malignant tumors. 31(4):731-8. Review.
(4) AJR 1984; Vanel D, et al. Pulmonary evaluation of patients with osteosarcoma: roles of standard radiography, tomography, CT, scintigraphy, and tomoscintigraphy. 143: 519-523
(5) Skeletal Radiol 1986; Rees CR, et al. The role of bone scintigraphy in osteogenic sarcoma. 15: 365-367
(6) Radiology 1980; 135: 177-180
(7) J Nucl Med 1990; Arrington ER, at al. Scintigraphic appearance of uncommon
soft-tissue osteogenic sarcoma metastases. 31: 679-681