Reflex Sympathetic Dystrophy:
(Sudeck's Atrophy)
Clinical
In the early stages of reflex sympathetic dystrophy (RSD) there is hyperaesthesia, pain, tenderness, swelling of the soft tissues, dystrophic skin changes, and vasomotor disturbances (cyanosis or erythema) in the affected limb. After 6 to 12 months the clinical picture becomes dominated by contractures and atrophy. RSD most commonly involves the hands and feet; shoulder pain and limitation of motion are seen in the shoulder-hand syndrome. Females are affected more commonly than males (3:1). Etiologies include local trauma (most common), immobilization, infection, post MI, post burn injury, or following a cerebral infarction.
Therapy is to treat the cause if known and to avoid immobilization at all costs. Early physical therapy is the key to a quick recovery. Steroids and sympathetic ganglion blockade can also be beneficial. The bone scan can also be used to predict a clinical response to treatment as about 90% of patients with a positive bone scan respond to steroid therapy (response rate among patients with negative scans is only 30%). Reversal of symptoms following sympathetic blockade can also be used to confirm the diagnosis of RSD.
Plain film findings in RSD include periarticular, mottled, irregular bony demineralization (seen in 30-60% of cases) and cortical thinning.
Scintigraphic Evaluation of RSD:
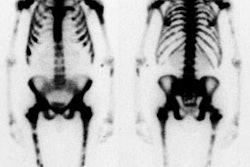
The 3 phase bone scan has a sensitivity of 96% and a specificity of 98% in detecting RSD. Clinically, RSD can be divided into early, mid, and late phases and the scintigraphic findings will vary depending upon the phase. A normal scan does not exclude the diagnosis of RSD.
Stage 1:
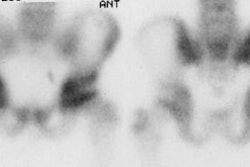
(Early 0 to 8-20 weeks) There is diffusely increase flow and blood pool activity in the affected extremity. Increased activity, particularly in a periarticular distribution is noted on delayed images. Decreased flow and blood pool activity may be seen uncommonly (1 to 8% of cases) particularly in young patients and hemiplegics [3].
Stage 2:
(Mid 2 to 6 months, possibly out to 1 year) Flow and blood pool abnormalities begin to normalize, but increased activity on delayed images persists.
Stage 3:
(Late Over 6 -12 months) Flow and blood pool activity can be normal or decreased (in about one-third of patients) in the involved extremity. Normal or decreased tracer activity are commonly seen on delayed images, although persistent increased delayed activity has been reported in up to 40% of patients [1]. Reduced flow in advanced RSD may be related to amyotrophia caused by disuse, which is a common feature of post-hemiplegic RSD. The decreased perfusion to the involved extremity also results in less tracer deposition.
In the evaluation of children for RSD increased activity on all 3-phases is seen in only 20% of cases. A pattern of decreased flow, blood pool, and delayed activity is more characteristically seen in children [2].
Following the initiation of early treatment, there is prompt normalization of flow and blood pool abnormalities, although persistent increased activity can be identified on delayed images.
REFERENCES:
(1) J Nucl Med 1998; Jan., p.29
(2) American Journal of Diseases of Children (AJDC) 1988; Silber TJ, Madj M. Reflex sympathetic dystrophy syndrome in children and adolescents. 142: 1325-1330
(3) J Nucl Med 1988; Demangeat JL, et al. Three-phase bone scanning in reflex sympathetic dystrophy of the hand. 29: 26-32