Performing a screening ultrasound exam along with mammography can yield breast cancer detection gains, but at the cost of a substantial increase in the number of false positives, according to findings from the American College of Radiology Imaging Network (ACRIN) 6666 screening ultrasound trial.
"The addition of a single screening ultrasonographic examination to mammography for women at elevated risk of breast cancer results in increased detection of breast cancers that are predominantly small and node-negative," wrote a research team led by Dr. Wendie Berg, Ph.D. (Journal of the American Medical Association, May 14, 2008, Vol. 299:18, pp. 2151-2163).
The ACRIN 6666 trial sought to compare the diagnostic yield of ultrasound and mammography with mammography alone, studying 2,809 women with an elevated breast cancer risk from 21 sites between April 2004 and February 2006. The 2,725 eligible patients in the study had heterogeneously dense breast tissue in at least one quadrant, and they were recruited to undergo mammographic and physician-performed ultrasonographic examinations in a randomized order by a radiologist blinded to the other examination results.
Women were excluded from the study if they had signs or symptoms of breast cancer. Other exclusion criteria included recent surgical or percutaneous image-guided breast interventional procedures, breast MRI or tomosynthesis within the previous 12 months, or mammography or whole-breast ultrasound within the previous 11 months. The researchers also excluded women with breast implants, those who were lactating, those who were planning to become pregnant within two years of the study, and those who had metastatic disease.
The women in the study had a mean age of 55.23 and a median age of 55. The researchers defined the reference standard as a combination of pathology and 12-month follow-up; results were available in 2,367 (96.8%) of the 2,725 eligible participants.
Of the patients included in the trial, 40 participants (41 breasts) received a diagnosis of breast cancer; whereas 39 actually had breast cancer. Six were ductal carcinoma in situ (DCIS), 20 were invasive ductal carcinoma (IDC) with or without DCIS, three were invasive lobular carcinoma, and 10 were mixed invasive ductal and lobular carcinoma with or without DCIS.
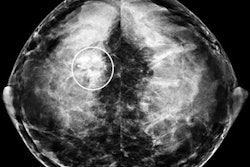
Eight cases were suspicious on both ultrasound and mammography, while 12 were suspicious on ultrasound alone. Eight participants (nine breasts) were suspicious on neither modality.
|
Of the 12 supplemental cancers detected by ultrasound alone, 11 (92%) were invasive with a median size of 10 mm (range 5-40 mm), and eight of the nine reported lesions had negative nodes.
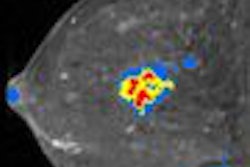
"Supplemental physician-performed screening ultrasound increases the cancer detection yield rate by 4.2 cancers per 1,000 women at elevated risk of breast cancer, as defined in this protocol (95% CI, 1.1-7.2 cancers per 1,000), on a single, prevalent screen," the authors wrote.
Increased false positives
Of the 2,637 study participants, 233 (8.8%) had findings considered suspicious on ultrasound; 136 had suspicious findings on ultrasound but not mammography. On the basis of ultrasound after full workup, 235 patients (8.9%) were recommended for biopsy.
However, only 20 (8.6%) of the 233 participants with suspicious ultrasound findings, 12 (8.8%) of the 136 patients with suspicious findings on ultrasound but not mammography, and 21 (8.9%) of the 235 patients who were recommended for biopsy based on ultrasound results were eventually found to have cancer.
Overall, the positive predictive value of biopsy recommendation after full diagnostic workup was 19 of 84 (22.6%) for the mammography group, 21 of 235 (8.9%) for ultrasound, and 31 of 276 (11.2%) for the combined mammography and ultrasound group.
"Adding a single screening ultrasound to mammography will yield an additional 1.1 to 7.2 cancers per 1,000 high-risk women but will also substantially increase the number of false positives," the researchers wrote.
Diagnostic uncertainty for complicated cysts remains a major source of false-positive results, with 43 participants undergoing only cyst aspiration included among those patients with suspicious false-positive results, according to the researchers.
The researchers also noted that their ongoing study, allowing for contrast-enhanced breast MRI within eight weeks of the final 24-month mammography and ultrasound screening round, may provide additional information on the possible competitive roles of MRI and ultrasound as adjuncts to mammographic screening. ACRIN 6666 is also continuing to evaluate annual screening ultrasound.
By Erik L. Ridley
AuntMinnie.com staff writer
May 13, 2008
Related Reading
Breast US boosts cancer detection, but with more false positives, November 26, 2007
US breast trial leaders aim to discuss ACRIN 6666 data at RSNA, October 8, 2007
Tumor type, breast profile determine value of mammo, US, and MR, January 6, 2005
Breast US readers need more practice with postop changes, December 22, 2004
Breast imagers fare better with hands-on approach to screening ultrasound, December 17, 2004
Copyright © 2008 AuntMinnie.com