Imaging facilities using breast MRI computer-aided detection (CAD) software say that insurance payors are declining to reimburse for the technology. The payment crunch could put the brakes on the growing use of breast MRI, and may make it more difficult for breast centers to meet rising demand.
A range of breast MRI facilities surveyed by AuntMinnie.com are reporting similar experiences: third-party payors are almost universally declining claims for breast MRI CAD procedures. Many industry observers believe the phenomenon is the unintended consequence of a reimbursement coding change for breast MRI exams using CAD that was implemented in 2006.
One breast MRI facility, First Hill Diagnostic Imaging of Seattle, has seen payors deny 483 claims for breast MRI exams under the new code between June 2006 and March 2008, according to medical director Dr. Bruce Porter. This represents a loss of more than $96,000 if the claims had been reimbursed in full.
"This is costing us many tens of thousands of dollars," Porter said. "I've spent years trying to train people on breast MRI, groups are having success in finding small cancers, and bam -- the rug is pulled out on one of the key tools."
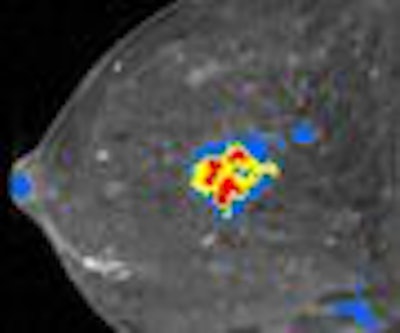
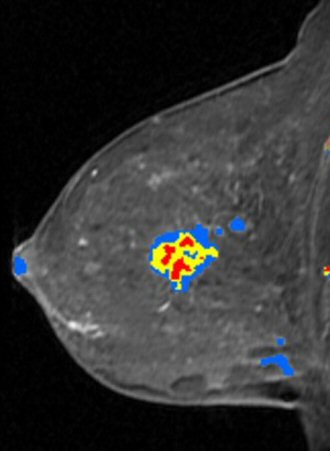 |
| Breast MRI advocates believe that CAD software saves time and makes images easier to interpret. Image courtesy of Confirma. |
An invaluable aid
Interest in breast MRI has been growing in recent years, particularly since the American Cancer Society (ACS) issued guidelines in 2007 recommending an annual breast MRI examination for the 1.4 million women believed to be at high risk for breast cancer.
But analyzing breast MRI exams can be a time-consuming process. While expert mammographers can analyze dozens of screening mammograms in an hour, a single breast MRI study has thousands of images and can take 30 minutes or more to review. Several companies have developed CAD software to help automate and speed up the process, including CAD Sciences of White Plains, NY; Confirma of Bellevue, WA; and Invivo of Orlando, FL.
Until 2006, facilities using breast MRI CAD submitted claims using Category I CPT codes: 3D reconstruction code 76377 and image subtraction code 76350 in conjunction with breast MRI codes 77058 (unilateral) or 77059 (bilateral). Breast MRI CAD claims were routinely being reimbursed by third-party payors at a rate of around $125 per exam.
But in 2005, CAD Sciences submitted a request to the American College of Radiology (ACR) of Reston, VA, for a new code specifically pertaining to breast MRI CAD. The good news is that the request was approved after the ACR submitted it to the American Medical Association (AMA), which manages CPT codes. The bad news is that the new code, 0159T, was established as a Category III code rather than a Category I code. Category III codes are reserved for emerging technologies to substantiate usage by clinicians, and have five years to transition into CPT I codes.
Confusion over the new code
|
Should you use CPT 0159T? CPT code 0159T covers the use of breast MRI CAD with "pharmacokinetic analysis." But only the CAD Sciences CAD software includes this feature. If you're using CAD software from another vendor, should you take your chances and bill under this code, or go with the Category I codes that prior to 2006 were being paid? The ACR advises that breast MRI sites only use CPT 0159T. While it may present short-term difficulties in getting paid, over the long term it will help establish breast MRI CAD and improve radiology's ability to get the technology converted into a Category I code. "Our official position is -- and always has been since we presented this code application to the CPT Editorial Panel -- that CPT III 0159T is to be used for any type of MRI CAD, whether it includes pharmacokinetic analysis or not," said Dr. Richard Duszak, chairman of ACR's Committee on Coding and Nomenclature. When radiologists don't report the code or report the wrong code, accurate data are never made available to the ACR and other breast imaging societies. This reduces the ACR's ability to act as physician and patient advocate to the AMA, according to Duszak. "If CAD is being performed 90% to 95% of the time with breast MRI, and becomes a de facto component of the standard of care, there may be a push at the CPT and RUC (RVS Update Committee) level to make this a combined code," Duszak said. "We are hearing this anecdotally, but must have data to determine the true co-incidence of these services so that we can move forward appropriately in the future and create a durable code. I would encourage everybody providing the service to bill for it." -- CK |
Computer aided detection, including computer algorithm analysis of MRI image data for lesion detection/characterization, pharmacokinetic analysis, with further physician review for interpretation breast MRI (list separately in addition to code for primary procedure).
In particular, some breast MRI users were confused by the inclusion of the pharmacokinetic analysis clause. Pharmacokinetic analysis is used by the CAD Sciences product, but not by the Confirma and Invivo software, raising the question of whether Confirma and Invivo customers should be using CPT code 0159T at all.
In addition, CPT code 0159T had not been assigned relative value units (RVUs), which are "weights" assigned to CPT codes that estimate the cost of providing a particular service, and which are used to calculate reimbursement within Medicare and other reimbursement fee schedules. No efforts were made to acquire a published non-Medicare RVU.
The upshot is that breast MRI facilities using the new code are being denied payment for CAD usage. Meanwhile, those facilities using the old code are also being denied payment because those codes have been superseded by the new code.
For the first six months of utilization, Medicare data showed 101 claims made between July and December 2006. Data for 2007 is not yet available. (Medicare data are presumed to seriously underestimate the number of breast MRI CAD exams being conducted because the overwhelming majority of the patient population receiving breast MRIs is under age 65.)
Health insurance companies have used the experimental nature of CPT code 0159T to avoid paying for breast MRI CAD, according to Porter. Radiologists interviewed for this article report that they are not receiving any reimbursement from local or national health insurance companies, in spite of major efforts to educate these companies on the costs and clinical value of breast MRI CAD.
Could facilities just continue submitting breast MRI CAD claims under the old Category I codes? They do so at their own peril. Consider the example of the Women's Center for Radiology in Orlando, FL.
The facility added breast MRI in October 2004 and pioneered the concept of breast MRI screening in Orange County, according to founder and medical director Dr. Susan Curry. When it started offering breast MRI, the center was scanning eight patients per day, a number that rapidly increased to 13 or more procedures daily.
Center manager Vicki Belmont said that before code 0159T went into effect, she submitted breast MRI CAD claims using codes 76377 and 76350, and for the most part was reimbursed an average of $125. In January 2007, Blue Cross Blue Shield of Florida asked the center to refund all image reconstruction and 3D payments made by the insurance company retroactive to October 2004, because it believed the codes were being used improperly.
The center requested a medical review board appeal, but this was denied by the insurance company. "We refunded Blue Cross Blue Shield of Florida the amount they requested, but we think that this was unfair," Curry said. "What would have been more equitable would have been returning payments made starting with our claims submitted after July 2006, when 0159T went into effect. We made an honest mistake by billing incorrect code, but since we have (Confirma's) CADstream, we did not think that 0159T applied to anyone but CAD Sciences customers."
Curry was not alone in her confusion. In an interview for this article with Henry Wyszomierski, CAD Sciences' vice president of corporate development, Wyszomierski stated, "It is not clear in my mind or anybody else's mind whether a Confirma system or an Invivo system qualifies under the new code. Even if the new code is moved along rapidly, it is not clear that the users of Confirma or Invivo can take advantage of it."
Dr. Michael Middleton, Ph.D., a faculty member and radiologist specializing in breast imaging of UCSD Hillcrest Department of Radiology in San Diego, was an early adopter of both breast MRI and breast MRI CAD. In 1992, he started performing breast MRI on women with breast implants. After interpreting 2,500 breast MRI examinations, he became one of the first radiologists in the U.S. to start using breast MRI CAD software.
"Breast MRI CAD makes me more efficient and also more accurate," Middleton said. "The CAD provides information that can automatically be gleaned from the data and presented to a radiologist in an organized way."
Middleton believes that the lack of reimbursement is going to make it more difficult for breast centers to provide a service that is experiencing growing demand within their communities. The timing is particularly sensitive as many facilities are already struggling under the reimbursement cuts of the Deficit Reduction Act of 2005.
"What many people do not realize is that each examination contains several thousand images, and that it is necessary to compare prior breast MRIs," he said. "This is very time-intensive to interpret, much more than other MRI procedures of other anatomy."
Both Middleton and Porter noted that many hidden costs to breast MRIs are not reimbursable. These include storage costs for the data-intensive files, and PACS networks and workstations that can support the retrieval and display of multiple prior breast MRI procedures. A radiologist shopping for CAD software who was interviewed for this article reported that the current price of breast MRI CAD software has been quoted to his hospital at $60,000 to $80,000. In addition to the initial capital investment, annual licensing fees and service contracts are necessary.
Dr. Michael Linver of X-Ray Associates of New Mexico in Albuquerque said that it's a contradiction for health insurance companies to pay for mammography CAD, but to deny payment for breast MRI CAD. The utility of CAD for conventional screening mammography has been well established in detecting early breast cancers, he noted. While suspicious lesions are visible with breast MRI, CAD software helps physicians interpret breast MRI studies with more confidence in less time.
"As a community practice, we need tools that will allow us to increase our study volumes to meet the growing demand," Linver said. "We do about eight breast MRIs a day, and with our other work, each of our mammographers is working at maximum capacity. Without breast MRI CAD, we would have to cut back on the number of breast MRI examinations we could offer at our center."
Possible solutions
Breast MRI advocates like Porter and Middleton are beginning a grassroots campaign to lobby third-party payors about the value of breast MRI CAD. The hope is that if one payor switches its policy others will fall into line.
Another tack is to have the ACR petition the AMA to switch code 0159T to Category I status, but it could take years for such a change to take effect. Even in a best-case scenario, a petition submitted in fall of 2008 wouldn't result in a category change until January 1, 2010, at the earliest, according to Michael Longacre, a reimbursement consultant with HealthCare Market Strategies of Yamhill, OR. In any event, no such application has been filed.
Another possibility would be to obtain a non-Medicare published resource-based relative value scale (RBRVS) unit for use with the 0159T code during the time period necessary to acquire a CPT 1 code, Longacre said.
"A CPT III code is problematic when it is not associated with corresponding published values for use by the payors when electronically processing the claim," he said. "Obtaining a non-Medicare published RBRVS value is a viable solution to this very serious problem."
Until then, breast MRI centers like First Hill Diagnostic Imaging, X-Ray Associates of New Mexico, and Women's Center for Radiology will have to question whether they can afford to continue to meet rising demand for breast MRI, especially as high-risk women begin seeking out the exam in response to the ACS guidelines.
"There are real costs associated with these CAD systems, and we aren't getting paid for them," First Hill's Porter said. "It has created a real disincentive for CAD."
By Cynthia Keen
AuntMinnie.com contributing writer
April 8, 2008
Related Reading
MRI beats mammography, US in detecting breast cancer in high-risk women, March 12, 2008
Catching undetected cancer with MR plus mammo in high-risk women outweighs costs, December 17, 2007
Breast MRI comparable to mammography for detecting later cancers, November 25, 2007
MRI beats US for breast screening of at-risk women, but yields more biopsies, August 6, 2007
ACS advocates breast MR screening for high-risk women, March 28, 2007
Copyright © 2008 AuntMinnie.com