A simple counting method that assesses coronary artery calcium (CAC) from low-dose chest CT scans can be used to predict an individual's risk of death from cardiac disease, according to study results published in the November issue of Radiology.
The method has broad potential to make better use of the high number of chest CT scans being acquired, particularly for lung cancer screening, the luminary research team from Tel Aviv, New York City, and three other U.S. centers reported.
Lung cancer screening programs are under way to study the benefit of early diagnosis of lung cancer, and the low-dose, ungated CT scans they produce can be used to simultaneously assess coronary artery calcification using an ordinal-visual scale, wrote study authors Joseph Shemesh, MD, from Sheba Medical Center in Tel Aviv, Israel, and Claudia Henschke, MD, from Mount Sinai School of Medicine in New York City; along with colleagues from Hadassah Medical Center in Jerusalem, Weill Cornell Medical College in New York City, and Arizona State University in Tempe.
Also, considering the release earlier this month of preliminary results from the National Lung Screening Trial (NLST) showing a clear mortality benefit in smokers and former smokers who undergo low-dose CT, screening programs are likely to move into the clinical mainstream within the next several years. A study presented in August warned that radiologists often ignore coronary artery calcium seen at low-dose chest CT.
"Even though the low-dose protocol was optimized for lung nodule detection, we found it reliable for CAC categorization of the four major Agatston score categories," Shemesh and colleagues wrote of their study. "Furthermore, the clinical value of this visual CAC score was found to be in accord with the results obtained by using the dedicated Agatston CAC score as generated with both electron-beam CT and multidetector-row CT" (Radiology, November 2010, Vol. 257:2, pp. 541-548).
Shemesh and colleagues sought to evaluate the usefulness of ordinal scoring of CAC by visual assessment at low-dose CT for predicting cardiovascular death. The researchers assessed the amount of coronary artery calcium on low-dose CT scans of the chest obtained between June 2000 and December 2005 in a cohort of 8,782 smokers ages 40 to 85 years.
These data were translated into the lifetime cumulative number of pack-years of cigarette smoking. For purposes of this analysis, categories for pack-years of smoking were as follows: less than 30 pack-years, 30 to 59 pack-years, and 60 pack-years or more. Categories of current smoking status were as follows: current smoker, quit within four years before enrollment, quit within five to 10 years before enrollment, or quit more than 10 years before enrollment.
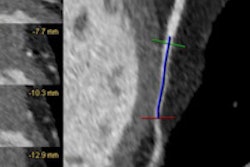
Each individual in the study underwent low-dose CT performed at 140 kVp or less and 80 mAs or less on a multidetector-row scanner in four institutions and a single-slice scanner in eight others. (The images were acquired between 2000 and 2005.) The section thickness was 1.25 mm or less for 2,640 scans, between 2 and 4 mm for 2,748 scans, and 5 mm in 3,394 scans.
To score the calcifications visually, the readers identified each of the four main coronary arteries, then categorized calcification from "mild" to "severe" and scored on a four-point scale (0-3), respectively. "Calcification was classified as mild when less than one-third of the length of the entire artery showed calcification, moderate when one-third to two-thirds of the artery showed calcification, and severe when more than two-thirds of the artery showed calcification," they wrote. Summing up the totals, each subject received a CAC score ranging from 0 to 12. The four categories of CAC used in the study were 0, 1-3, 4-6, and 7-12.
Information on deaths was obtained from the National Death Index, and the researchers calculated follow-up time (median, 72.3 months; range, 0.3-91.9) as the time between CT and death, loss to follow-up, or the end of the analysis at December 31, 2007, whichever came first.
The results showed rising rates of cardiovascular deaths with increasing CAC scores:
- 1.2% (43 of 3,573 subjects) for a score of 0
- 1.8% (66 of 3,569 subjects) for a score of 1-3
- 5.0% (51 of 1,015 subjects) for a score of 4-6
- 5.3% (33 of 625 subjects) for a score of 7-12
Using a zero CAC score as the reference group, a CAC score of at least four was a significant predictor of cardiovascular death (odds ratio = 4.7; 95% confidence interval: 3.3-6.8; p < 0.0001). Even when adjusted for sex, age, and pack-years of smoking, the CAC score remained significant (odds ratio = 2.1; 95% confidence interval: 1.4-3.1; p = 0.0002).
"Our results suggest that quantitative assessment of the extent of coronary calcifications should be made on all CT scans of the chest because it provides relevant prognostic information, even when using an ordinal scale," Shemesh and colleagues concluded. "This suggestion is particularly relevant for low-dose CT screening programs of asymptomatic people at risk for both diseases because of smoking."
One large cancer screening takes an alternative approach to the same end by using a single ungated low-dose CT scan of the chest to identify both CAC and lung cancer -- an approach that reduces radiation exposure and costs by using a single scan rather than two separate scans, they added.
Citing limitations to the study, the authors said they were unable to assess the Framingham cardiovascular risk because participants in the lung cancer screening program did not fully register this information at baseline. In addition, the effect of CAC on acute myocardial infarction was not assessed. Current recommendations call for performing low-dose coronary CT to determine the CAC score in asymptomatic subjects with intermediate Framingham cardiac risk (recommendation class IIA or IIB) to refine the risk assessment and adjust the intensity of treatment.
However, they added, studies that have assessed both CAC and risk factors have "consistently demonstrated the independent and incremental prognostic value of CAC measurement over the Framingham risk stratification for cardiac events and all-cause mortality."
By Eric Barnes
AuntMinnie.com staff writer
November 24, 2010
Related Reading
CT calcium scoring alters cardiac risk estimates, October 10, 2010
SHAPE II task force revising cardiac risk guidelines, August 17, 2010
Coronary calcium usually ignored on chest CT, August 12, 2010
Coronary calcium score doesn't help predict risk in low-risk men, June 7, 2010
CT equivalent to IVUS for culprit plaque detection, December 4, 2008
Copyright © 2010 AuntMinnie.com