Radiologists already have access to computer-aided detection (CAD) software for analyzing medical images. But what if you had a tool that provides an extra level of data analysis including patient demographic risk factors and outcomes data? Would it help you decide whether a finding warranted recalling the patient?
Researchers from the University of Wisconsin in Madison have developed just such a tool, which they believe could prove useful as a decision-support aid for radiologists reviewing mammograms. They found that the algorithm produced statistically significant increases in sensitivity and specificity when compared with radiologists working without it, according to a paper published online April 14 in Radiology.
Dr. Elizabeth Burnside, assistant professor of radiology, was inspired 10 years ago to find a way to use the data being electronically accrued in cancer registries and mammography information systems. In 2004, Burnside collaborated with C. David Page, Ph.D., a professor in the University of Wisconsin's department of biostatistics and medical informatics, and the two began to develop decision models and machine-learning applications.
The researchers ultimately developed a software algorithm that takes information from a radiology report and compares it against a database of 62,000 final reports of malignant and benign findings.
For example, if a radiologist singles out an area on a mammogram as being suspicious, the algorithm compares demographic data for that patient against demographic and outcomes data in the database for patients with a similar background. The software then makes a recommendation as to the level of risk the patient has of having breast cancer, which the radiologist can use in determining whether to recall the patient.
Burnside and Page pointed out that the algorithm is not CAD, in that it doesn't analyze medical images the way that CAD software does. In addition, the algorithm isn't used to locate occult findings, but rather to analyze findings that have already been discovered. But it does make use of Bayesian network analysis, a method for analyzing variables and probabilities that sometimes is used in CAD applications.
Testing it out
To test the software, the team used a database of screening and diagnostic mammography exams performed between April 1999 and February 2004 at Froedtert and Medical College of Wisconsin Breast Care Center in Milwaukee. In addition to patient demographic information, the database contained 48,744 structured reports (Mammography Information System, PenRad Technologies, Minnetonka, MN) of mammography exams of 18,269 patients.
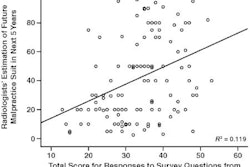
The researchers first calculated the sensitivity and specificity of the radiologists working without benefit of the algorithm. They then analyzed the original reports with the Bayesian network algorithm to determine its effect had it been in clinical use at the time, calculating cancer detection rate, early-stage cancer detection rate, and abnormal interpretation rate.
Receiver operator characteristics (ROC) curves were constructed, and baseline sensitivity and specificity of the individual radiologists and the radiologists as a group were calculated. A total of 62,219 findings were analyzed, of which 510 findings represented malignancies and 61,709 findings were benign or negative.
The cancers included masses, microcalcification asymmetries, and architectural distortions. Findings were identified in all types of tissue: 14% in predominantly fatty tissue, 41% in scattered fibroglandular tissue, 36% in heterogenously dense tissue, and 8% in extremely dense tissue.
In analyzing the data, the researchers found that the algorithm would have improved the sensitivity and specificity of the radiologists by five percentage points. In their original analysis of the mammograms, the radiologists detected 8.9 cancers per 1,000 mammograms and had an abnormal interpretation rate of 18.5%, with a sensitivity of 85.3% and a specificity of 88.1%. Adding Bayesian network analysis increased sensitivity to 90.0% and specificity to 93.0%.
Real-world usage
In real-time usage envisioned for the future, a radiologist would provide observations and assessments that the Bayesian network would combine with knowledge of similar past findings to generate accurate predictions of malignancy.
The algorithm's strength as a risk prediction model is that it estimates breast cancer risk at a particular point in time. Its weakness is that its analytic capability is based on the lexicon terminology and the description of findings contained in the structured report, which may lack detail, be inaccurate, or vary between radiologists.
In this evaluation, the Bayesian network was most effective in decreasing the need for recall, according to its developers. During its testing, the Bayesian network classified thousands of false-positive BI-RADS category 0 assessments correctly as negative.
The inability to account for a huge number of dependencies between predictive variables, such as microcalcification types, mass types, associated findings, and demographic risk factors, without a computer's calculation assistance may account for some radiologist errors and performance variability, according to Burnside.
Future developments
After additional validation testing, the next step will be to integrate the decision-support tool with a mammography information system, Burnside and Page told AuntMinnie.com. Although the algorithm's calculations take less than one second for each patient, data have to be entered into a separate database, which is unnecessarily time consuming and would disrupt the workflow of the interpreting radiologist.
A multi-institutional prospective study is planned in the near future, ideally after integration between the Bayesian network and the mammography information system has been achieved.
A more sophisticated version of the decision-support tool is in development, Page said, and is based on statistical relational learning. It will be able to analyze a wide variety of data types in its predictive model, potentially including individual DNA or data from images.
"The current software makes predictions based on fairly well known predictive features like mass size, mass density, and calcification shape of an identified abnormality. The software in development will be able to take into account features such as a change in the properties of a known abnormality as compared to the last mammogram," Page explained.
Using inductive logic programming, the new software also can identify previously undiscovered risk factors. The capability of searching through millions of possible combinations of risk factors and identifying those which are viable enable it to continue expanding the risk factor database.
"Our objective is to develop a tool that will enhance the expertise of the radiologist. Ideally, the radiologist and computer would work as collaborative partners to manage the huge amount of predictive information available at the time of mammography to accurately assess breast cancer risk," Burnside said.
By Cynthia E. Keen
AuntMinnie.com staff writer
April 20, 2009
Copyright © 2009 AuntMinnie.com