One of the manifestations of borderline personality disorder (BPD) is the repeated self-infliction of pain. BPD patients often describe a sense of emotional release and relief when they engage in such destructive activities as cutting their flesh, burning their skin, or hitting themselves. A new study used functional MRI (fMRI) to gain insight into the neurological pain response of BPD patients who partake in self-injurious behavior.
"Patients with BPD frequently experience stress-induced aversive states of reduced pain perception and dissociation, which are often relieved by self-injurious behavior," wrote Dr. Christian Schmahl and colleagues. "It can be assumed that disturbed affective pain components or disturbed pain control mechanisms underlie reduced pain perception in patients with BPD" (Archives of General Psychiatry, June 2006, Vol. 63:6, pp. 659-667).
Schmahl is from the Central Institute of Mental Health in Manheim, Germany. His co-authors are from various institutions in Germany, Italy, and Switzerland. Co-investigators Drs. Klaus Scheffler and Juergen Hennig are from the department of radiological research-medical physics at the University of Freiburg in Germany.
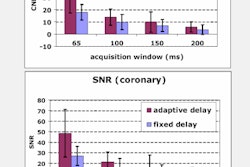
For this study, 12 women with BPD who reported self-injurious behavior (cutting, burning) and 12 age-matched healthy controls underwent fMRI while painful heat stimuli were applied to their hands. The heat stimuli were delivered using a thermode with temperatures oscillating from 40° Celsius to 48° Celsius.
Patients were imaged in two different 1.5-tesla scanners (Sonata or Vision, Siemens Medical Solutions, Erlangen, Germany). Whole-brain structural volumes were acquired with a T1-weighted, 3D, magnetization-prepared, rapid-acquisition gradient-echo sequence. The blood oxygen level-dependent (BOLD) signal was acquired using gradient-recalled echo-planar imaging.
According to the fMRI results, both groups showed a consistent pattern of regional signal increases during various temperature conditions. The two groups revealed bilateral activation in the secondary somatosensory cortex. In the medial pain system, the medial thalamus was activated bilaterally in patients and contralaterally in controls. In the dorsolateral prefrontal cortex (DLPFC), the activation pattern differed between the two groups.
Finally, significant decreases in the BOLD signal were found in the perigenual anterior cingulated cortex (ACC) and the amygdala of the BPD subjects. These two areas of the brain regulate the emotional evaluation of pain.
"Contrasting brain activity between patients and controls, we found differences in the activity of the DLPFC, PPC (posterior parietal cortex), ACC, and amygdala," the authors summarized. "Patients with BPD ... displayed a significant reduction in pain sensation and a dissociable neural response in brain areas concerned with cognitive and emotional evaluation of pain."
The authors noted that both groups showed an activation of pain pathways, but that the BPD patients had a different pattern of activation, which may indicate a circuit of pathologically reduced pain perception.
Based on this data, the group came to two main conclusions as to why and how some BPD patients chronically injure themselves. First, self-inflicted pain may function to normalize neural activity in the regions that are responsible for emotional and cognitive processing (i.e., the sense of release). Also, repeated self-injury could lead to an adaptation of pain thresholds and pain processing. These processes combined allow self-injuring BPD patients to down-regulate the emotional components of pain and continue to seek out painful experiences.
By Shalmali Pal
AuntMinnie.com staff writer
June 28, 2006
Related Reading
Brain imaging predicts treatment success in depressed patients, April 12, 2006
MRS detects positive neuronal changes in ex-meth abusers, May 6, 2005
Copyright © 2006 AuntMinnie.com